INSIDE
The first five years ANMF’s National Policy Research Unit reflects how research is integral to members and the community
International recruitment Can it be tackled ethically amid a global workforce shortage?
Attention to climate change The responsibility of nurses and midwives to take action and improve health outcomes

ANMF PRIORITIES 2023 A PUBLICATION OF THE AUSTRALIAN NURSING AND MIDWIFERY FEDERATION VOLUME 27, NO.10 JAN–MAR 2023
When they put their trust in you, it’s vital to have information you can trust )





Be up to date with the 2023 AMH Book or Online







We are constantly improving and updating the AMH. Here are some examples of the recent changes that may interest you:

• COVID-19 updates, including more detail on COVID-19 vaccines and the oral treatments molnupiravir and nirmatrelvir with ritonavir





• new monographs, eg eptinezumab for migraine prevention, diroximel fumarate for MS














• revised therapeutic information, eg for psoriasis, heart failure, stroke
• many new and revised drug interactions, eg aspirin + NSAIDs




There is a summary of key changes, including all new and deleted drugs, in every edition. The 2023 AMH is available in hard copy, online or available as an APP download to PC’s, Surface Pros and Mac computers for of ine use with Ctrl F search capability. To access full content a subscription is required.

For more information go to www.amh.net.au
 Butler ANMF Federal Secretary
Butler ANMF Federal Secretary
The start of a new year often permits us to press the reset button, whether it’s setting new intentions, learning from the past or growing on the back of our achievements.
For the ANMF, the New Year is an opportunity to reflect on our wins, plan how to build on our successes and strategise where our focus is needed during 2023.
Towards the end of last year, we finally saw landmark legislation ensuring a registered nurse on-site and on duty 24/7 in all aged care facilities. The legislation also requires care providers to be more transparent and accountable regarding their use of taxpayer funding.
Further, the Government made a commitment to mandate the number of care minutes residents receive as part of its $3.9 billion aged care reform package.

While last November, the ANMF and HSU also secured an interim 15% pay rise for aged care workers through the Fair Work Commission.
These reforms will significantly strengthen the sector and will start to address much of the chronic understaffing.
The ANMF will work with key stakeholders to ensure these legislated changes will be applied when they are due to be implemented during 2023/4.
The union will also advocate for reducing public hospital admissions from aged care by increasing and embedding Residential In Reach (RIR) teams in public health services to meet local demand.
Further, the ANMF will push to mandate skill mix percentages or RN/EN/PCA care minutes and will lobby for better career pathways into and within aged care, including expanding the NPs role in aged care via a national plan.
Chronic staff shortages exacerbated by the pressures of COVID-19 over the past two years have created significant issues impacting all sectors.
Nurses and midwives across the board have reported feeling overwhelmed, anxious and exhausted, under the extreme conditions they work in day to day.
Many have reported the need for safe workloads, minimum staff ratios and skills mix, paid overtime, wage increases and safe working environments.
The ANMF is advocating to improve these essential conditions and will push for nurses and midwives to work to their full scope of practice, including the introduction of innovative models of care to reduce the burden.
Importantly, we will be working on effective recruitment and retention practices of nurses, midwives and qualified care workers to help further reduce the strain of the system in crisis.
This includes working with the government, alongside the Council of Deans of Nursing and Midwifery (Australia and New Zealand), the Nursing and Midwifery Board of Australia (NMBA), the Australian and Nursing Midwifery Accreditation Council (ANMAC) and other peak nursing bodies on strategies to grow our nursing, midwifery and care worker workforce and ensure a sustainable pipeline for the future.
Industrial relations reform will make up a significant part of the ANMF’s work this year.
This includes creating less burdensome threshold requirements for taking protected industrial action; advocating for permanent employment and only limited use of fixed-term contracts, and keeping pressure on employers to comply with flexible working arrangement obligations rather than relying on casual work arrangements.
These priorities are just a few the ANMF will pursue during 2023. To read about these and others in detail, turn to this issue’s feature on page 8.
After many challenges, highs and lows over the past 12 months, the ANMF is ready and eager to advocate for better conditions for all our members. Working as a collective, we are unstoppable and will achieve the critical outcomes necessary to provide the care Australians deserve.
Importantly, we will be working on effective recruitment and retention practices of nurses, midwives and qualified care workers to help further reduce the strain of the system in crisis.
EDITORIAL Jan–Mar 2023 Volume 27, No. 10 1
Annie
ANMF FEDERAL & ANMJ
Level 1, 365 Queen Street, Melbourne Vic 3000 anmffederal@anmf.org.au
To contact ANMJ: anmj@anmf.org.au
FEDERAL SECRETARY
FEDERAL ASSISTANT SECRETARY



ACT
NT
SA
OFFICE ADDRESS 2/53 Dundas Court, Phillip ACT 2606
POSTAL ADDRESS PO Box 4, Woden ACT 2606 Ph: 02 6282 9455 Fax: 02 6282 8447 anmfact@anmfact.org.au
OFFICE ADDRESS
16 Caryota Court, Coconut Grove NT 0810
POSTAL ADDRESS PO Box 42533, Casuarina NT 0811 Ph: 08 8920 0700 Fax: 08 8985 5930 info@anmfnt.org.au
OFFICE ADDRESS
191 Torrens Road, Ridleyton SA 5008
POSTAL ADDRESS
PO Box 861 Regency Park BC SA 5942 Ph: 08 8334 1900 Fax: 08 8334 1901 enquiry@anmfsa.org.au
OFFICE ADDRESS
535 Elizabeth Street, Melbourne Vic 3000
POSTAL ADDRESS PO Box 12600, A’Beckett Street, Melbourne Vic 8006 Ph: 03 9275 9333 / Fax: 03 9275 9344 MEMBER ASSISTANCE anmfvic.asn.au/memberassistance
OFFICE ADDRESS
50 O’Dea Avenue, Waterloo NSW 2017 Ph: 1300 367 962 Fax: 02 9662 1414 gensec@nswnma.asn.au
OFFICE ADDRESS
106 Victoria Street West End Qld 4101
POSTAL ADDRESS GPO Box 1289 Brisbane Qld 4001 Phone 07 3840 1444 Fax 07 3844 9387 qnmu@qnmu.org.au
TAS
OFFICE ADDRESS
182 Macquarie Street Hobart Tas 7000 Ph: 03 6223 6777 Fax: 03 6224 0229







Direct information 1800 001 241 toll free enquiries@anmftas.org.au
OFFICE ADDRESS 260 Pier Street, Perth WA 6000
POSTAL ADDRESS PO Box 8240 Perth BC WA 6849 Ph: 08 6218 9444 Fax: 08 9218 9455 1800 199 145 (toll free) anf@anfwa.asn.au
BRANCH SECRETARY
Matthew Daniel
BRANCH SECRETARY
Cath Hatcher
BRANCH SECRETARY Elizabeth Dabars
VIC
BRANCH SECRETARY Lisa Fitzpatrick
NSW
BRANCH SECRETARY
Shaye Candish
QLD BRANCH SECRETARY Beth Mohle
BRANCH SECRETARY Emily Shepherd
WA BRANCH SECRETARY Janet Reah
Annie Butler
Lori-Anne Sharp DIRECTORY
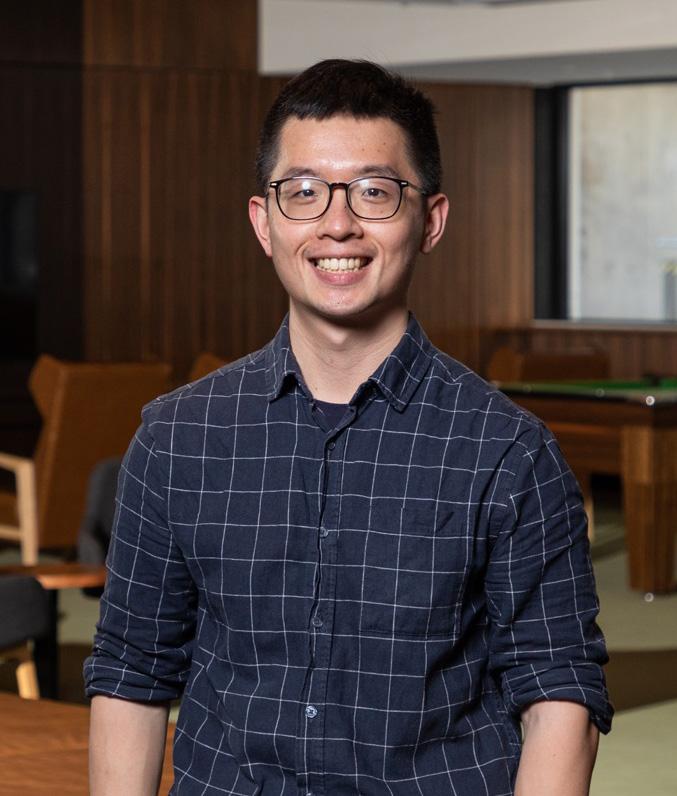
Front cover
Advanced Practice Nurse Alison Wong, ED Nurse Practitioner Stuart Smith and Palliative Care Nurse Practitioner Juliane Samara
 Image by Lydia Downe
Image by Lydia Downe
Editorial
Editor: Kathryn Anderson Journalist: Robert Fedele Journalist: Natalie Dragon Production Manager: Cathy Fasciale Level 1, 365 Queen Street, Melbourne Vic 3000 anmj@anmf.org.au
Advertising Heidi Hosking heidi@anmf.org.au 0499 310 144
Design and production
Graphic Designer: Erika Budiman instagram.com/pixels_and_paper_studio
Printing: IVE Group Distribution: D&D Mailing Services
The Australian Nursing & Midwifery Journal is delivered free quarterly to members of ANMF Branches other than New South Wales, Queensland, Western Australia and ACT. Subscription rates are available via anmjadmin@anmf.org.au. Nurses and midwives who wish to join the ANMF should contact their state or territory branch. The statements or opinions expressed in the journal reflect the view of the authors and do not represent the official policy of the Australian Nursing & Midwifery Federation unless this is so stated. Although all accepted advertising material is expected to conform to the ANMF’s ethical standards, such acceptance does not imply endorsement. All rights reserved. Material in the Australian Nursing & Midwifery Journal is copyright and may be reprinted only by arrangement with the Australian Nursing & Midwifery Journal
Note: ANMJ is indexed in the cumulative index to nursing and allied health literature and the international nursing index ISSN 2202-7114 Online: ISSN 2207-1512
Moving state?
Transfer your ANMF membership
If you are a financial member of the ANMF, QNMU or NSWNMA, you can transfer your membership by phoning your union branch. Don’t take risks with your ANMF membership – transfer to the appropriate branch for total union cover. It is important for members to consider that nurses who do not transfer their membership are probably not covered by professional indemnity insurance.
ANMJ is printed on A2 Gloss Finesse, PEFC accredited paper. The journal is also wrapped in biowrap, a degradable wrap.
The ANMJ acknowledges the Traditional Owners and Custodians of this nation. We pay our respects to Elders past, present and emerging. We celebrate the stories, culture and traditions of Aboriginal and Torres Strait Islander Elders of all communities. We acknowledge their continuing connection to the land, water and culture, and recognise their valuable contributions to society.
FEATURE 8
CLINICAL
16 Seeing the opportunity: Increasing the potential for eye donation 32 A clinical pathway for management of
related behaviours in RACFs FOCUS 43 Undergraduate nursing & midwifery students and graduate transition to practice
REGULAR COLUMNS 1 Editorial 2 Directory 4 News Bites 6 Lori-Anne 14 James 20 Environment 23 Legal 24 International 28 Research 30 Professional 31 Working Life 34 Industrial 36 Reflection 38 Issues 39 Research & Policy 40 Viewpoint 56 Healthy Eating
ANMF Priorities 2023
UPDATES
dementia
8
VOLUME
@ANMJAUSTRALIA ANMJ.ORG.AU
JAN–MAR 2023
27, NO.10
CONTENTS
Night owls beware: Bedtime procrastination impacts wellbeing

Bedtime procrastination correlates with increased daytime fatigue, shorter sleep duration and lower sleep quality.
New national centre on women’s mental health
A new national centre that addresses women’s mental health throughout all life stages has been launched.
The HER Centre for Women’s Health, based at Monash University, conducts research, treats women and improves awareness about women’s mental health issues occurring at all ages.
Women experience nearly twice as much depression as men, four times as much anxiety and 12 times the rate of eating disorders. Their mental illness involves a complex interaction of biological, psychological, and social factors, of which the causes of, and best treatments for, conditions such as depression, anxiety, trauma disorders, addictions, and self-harm are different to men’s.
HER Centre Director and Head of the Department of Psychiatry at Monash University, Professor Jayashri Kulkarni said for too long women’s mental health problems had been underdiagnosed and, in some cases, unrecognised.

“What we now know is, and science has told us, that many women of all ages are living with mental illnesses that may be related to female hormones and/or other parts of their biology.
According to CQUniversity (CQU) research, bedtime procrastination is prevalent with more than 50% of adults indicating they go to bed later than intended three or more days a week.
“Bedtime procrastination is the intentional delay of going to bed, without any external circumstances causing the delay - such as children, pets, or being on call for work,” CQU PhD candidate Vanessa Hill said.
“Many people procrastinate their bedtime from time to time, though for some people this is a regular occurrence that has a severe impact on their daily wellbeing. The results show that higher bedtime procrastination is correlated with shorter sleep duration, lower sleep quality and increased daytime fatigue.”
Higher bedtime procrastination correlated with lower selfcontrol and evening chronotype (night owls).
Bedtime procrastination is a growing area of research, with 55% of articles included in the systematic review published in 2020-2021.
“These results are an important first step for scientists to develop interventions to promote adequate sleep for people who have bedtime procrastination problems. For others who want to improve their overall health, this research shows that procrastinating bedtime could have a negative impact on their sleep,” Ms Hill said.
The study, ‘Go to bed! A systematic review and meta-analysis of bedtime procrastination correlates and sleep outcomes’ is published in Sleep Medicine Reviews
“A woman can experience pre-menstrual or menopause-related depression that is as serious as any other type of depression. Yet it can be easily written off as part of a ‘normal’ hormonal cycle. At its worst, such conditions can lead to serious mental illness or even suicide, without the true cause being identified.”
Environmental factors that impact many women and can contribute to mental ill health include experiencing violence, power imbalance, lower wages, and negative cultural expectations. Researchers in HER Centre are currently working on hormonebased treatments for women with menopausal depression. Clinical trials are also underway that are treating women with new forms of oestrogen, while educating health professionals about the need for them and their worth.
Visit: monash.edu/medicine/her-centre
NEWS BITES 4 Jan–Mar 2023 Volume 27, No. 10
HER Centre Australia launch Jo Stanley (L) with Director Jayashri Kulkarni
NEW FUNDING TO ADDRESS INSTITUTIONAL RACISM IN AUSTRALIA’S HEALTHCARE SYSTEM
A new National Health and Medical Research Council (NHMRC) Synergy Grant of $5 million over five years will help to reform the delivery of hospital care for Aboriginal and Torres Strait Islander peoples by addressing implicit bias and institutional racism within Australian hospitals.
Associate Professor and Waljen woman Tamara Mackean from the Guunumanaa (Heal) Aboriginal and Torres Strait Islander Health Program at The George Institute will lead the collaboration between Aboriginal and Torres Strait Islander and non-Indigenous researchers. The grant will look to understand and address the complex dynamics of racism, implicit bias and colonisation which
significantly impact the health and wellbeing of Aboriginal and Torres Strait Islander people and families.
“This project is focused on structural reform as a necessary part of healing for Aboriginal and Torres Strait Islander people and families who have suffered ongoing trauma and injustice within the health system,” Associate Professor Mackean said.

The team will “bring Aboriginal and Torres Strait Islander knowledge of health and healing alongside Western biomedical knowledge to produce new meaning based on mutual respect,” Associate Professor Mackean said.
10 minutes of aerobic exercise with exposure therapy reduces PTSD symptoms
A short burst of aerobic exercise could promote a molecule in the brain that is crucial for learning to feel safe, according to a new study.
Exposure therapy is one of the leading treatments for post-traumatic stress disorder (PTSD), yet, up to half of all patients don’t respond to it.
But now, a study led by UNSW Sydney psychologists has found that augmenting the therapy with 10 minutes of aerobic exercise has led to patients reporting greater reduction to PTSD symptom severity six months after the nine-week treatment ended.
In the first known single-blind randomised control trial of its kind, researchers in Sydney recruited 130 adults with clinically diagnosed PTSD and assigned them to two groups. People in both groups received nine 90-minute exposure therapy sessions. At the end of each session, one group was put through 10 minutes of aerobic exercises, while members of the control group were given 10 minutes of passive stretching.
Findings, published in The Lancet Psychiatry, showed people in the aerobic exercise group on average reported lower severity of PTSD symptoms – as measured on the CAPS-2 scale – than those who had their exposure therapy augmented by stretching exercises at the six-month follow-up.

The goal of exposure therapy in treating PTSD is extinction learning, where a patient learns to equate something that up until now they have associated with trauma, with a feeling of safety.
Of note, there were no clear differences between the two groups one week after the treatment program ended, suggesting the benefits take time to develop.
More people seeking care at emergency departments, report shows
Public emergency departments (EDs) across Australia saw the highest number of patient presentations in 2020-21, a new report by the Australasian College of Emergency Medicine (ACEM) has revealed.
The finding was one of many in State of Emergency 2022 (SOE22) an inaugural annual report consisting of data from Australian public major, metropolitan, and regional hospitals.
The report shows that demand for emergency care has risen by 14% since 2016-17 – despite the population only growing by 5% – and that patients needing hospital admission were stuck waiting five hours longer than safe recommended targets for a bed, or an average wait of almost 13 hours.
According to ACEM, the data suggests the pressures were not caused by the COVID-19 pandemic and have instead been steadily increasing for years.
The report provides detailed insights into how many people present to EDs for mental health support, the busiest time and day in EDs, how long people are waiting for care, or a bed, and how many people give up and leave before even receiving treatment.
It also makes recommendations for strategic nationwide approaches to reduce pressures on EDs and the broader health system.
“EDs in every state and territory in Australia are in a state of emergency. There have never been more people requiring acute healthcare, people have never had such complex health needs, and people have never had to wait so long for urgently needed care,” ACEM President Dr Clare Skinner said.
Associate Professor Tamara Mackean
Photo:The George Institute for Global Health
NEWS BITES Jan–Mar 2023 Volume 27, No. 10 5
Sharp ANMF Federal Assistant Secretary
More cake this festive season?
As we start a fresh year, I am continuing my long-standing tradition by sharing one of my favourite recipes in the Jan-Mar issue of the ANMJ.
If you have read my columns over the years, you may have gathered I have a passion for cooking and delight in sharing food with family, friends and colleagues. What you may not know is that I also love gardening and like nothing more than growing and sharing fresh produce from the backyard veggie patch.

At a recent social gathering, The Honourable Nicola Roxon (now chair of HESTA -Industry Super Fund) brought her delicious rhubarb and cinnamon cake.
Because I have an abundance of rhubarb growing in my garden, Nicola graciously shared her recipe with me.
The cake I baked was just as delectable as Nicola’s and was greatly enjoyed by family and friends. If you get the time to try it, I promise it will not disappoint.
Nicola’s rhubarb and cinnamon cake

INGREDIENTS
Batter
80g butter
300g brown sugar
2 eggs
1 tsp vanilla
300g flour
1 tsp bicarbonate soda
500g rhubarb stalks, sliced into 1 cm pieces, or add apple or pear to bulk up if needed
METHOD
250g full cream sour cream or thick yoghurt
Grated lemon zest
Topping
80g brown sugar 1 tsp cinnamon
1. Preheat oven to 180�C. Grease and line a deep rectangular cake tin (approximately 33 x 23 cm).
2. Cream together the butter and brown sugar.
3. Add the eggs and vanilla, and then fold in the sifted flour and bicarbonate soda.
4. Stir in the sour cream and zest, and once combined add the rhubarb pieces.
5. In a small bowl, mix together the brown sugar and cinnamon for the topping.
6. Pour the batter into the cake tin and finally, sprinkle the topping over the top of the batter.
7. Bake for at least 50–60 minutes. Test with a skewer, and continue to bake until skewer comes out cleanly.
8. Best served with crème fraiche or vanilla ice cream.
There is nothing like using ingredients you have grown yourself and always so much easier when you have it at the back doorstep, avoiding that last minute rush to the shops for ingredients. This year to my delight, my love, nurturing and hard work in the garden paid off, resulting in a bumper crop of rhubarb perfect for this cake.
After tasting the cake, my family and friends agreed my efforts at growing rhubarb was well worth it.
Nicola has kindly allowed me to share her rhubarb and cinnamon cake with you. I hope you enjoy it as much as I do.
Lori-Anne
instagram.com/pixels_and_paper_studio LORI -ANNE 6 Jan–Mar 2023 Volume 27, No. 10
Food styling and photo by Erika Budiman ©
Move to Maltofer®
Maltofer ® restores iron levels with significantly less constipation and better treatment compliance than ferrous sulfate.1–3
Maltofer® contains iron as iron polymaltose. For more information visit maltofer.com.au *In a study comparing iron polymaltose with ferrous sulfate in iron deficient pregnant patients. n=80.

References: 1. Ortiz R et al. J Matern Fetal Neonatal Med 2011;24:1–6. 2. Toblli JE & Brignoli R. Arzneimittelforschung 2007;57:431–38. 3. Jacobs P et al. Hematology 2000;5:77–83. Healthcare professionals should review the full product information before recommending, which is available from Vifor Pharma on request.
Maltofer is for the treatment of iron deficiency in adults and adolescents where the use of ferrous iron supplements is not tolerated, or otherwise inappropriate. For the prevention of iron deficiency in adults and adolescents determined by a medical practitioner to be at high-risk, where the use of ferrous iron supplements is not tolerated, or otherwise inappropriate. If you have iron deficiency, your doctor will advise you whether an oral iron treatment is required.
Maltofer® is a registered trademark of Vifor Pharma used under licence by Aspen Pharmacare Australia Pty Ltd. For medical and product enquiries, contact Vifor Pharma Medical Information on 1800 202 674. For sales and distribution enquiries, contact Aspen Pharmacare customer service on 1300 659 646. AU-MAL-1900004. ASPHCH1150/ANMJ. Date of preparation August 2019.

Fewer pregnant women experience constipation with Maltofer ®1* Maltofer® 2% of patients Ferrous sulfate 23% of patients IS THEIR IRON CAUSING CONSTIPATION? Up to 54% of patients studied did not complete their full course of ferrous sulfate as prescribed.1*
ANMF PRIORITIES 2023
On the back of a positive 2022 with action to start improving conditions in our health, aged care and welfare sectors, the ANMF is determined to work on a list of priorities over 2023 that will support the professions and the health systems they work in. ROBERT FEDELE and NATALIE DRAGON report.
 Advanced Practice Nurse Alison Wong, ED Nurse Practitioner Stuart Smith and Palliative Care Nurse Practitioner Juliane Samara lobbying politicians in Canberra last October.
Photo: Lydia Downe
Advanced Practice Nurse Alison Wong, ED Nurse Practitioner Stuart Smith and Palliative Care Nurse Practitioner Juliane Samara lobbying politicians in Canberra last October.
Photo: Lydia Downe
FEATURE
Gender equity
Australia is one of the few developed nations that does not actively set targets for gender equality. Yet, Australian women experience inequality in many areas of their working and social lives, including disparate wages, poverty, discrimination and gender-based violence.

Recent statistics show that the Australian gender pay gap is currently at 17.2%, which means females only earn 83 cents for every dollar earned by males.
Post-COVID, Australia has further slid down the rankings in the World Economic Forum’s Global Gender Gap Index to 50TH , down from 44TH in 2020 and 15TH when the index first launched. Australia is lagging in ‘economic participation and opportunity’ in women’s labour force participation rate, wage equality and earned income.
The Government’s plan for boosting wages in female-dominated industries will go some way to improving gender equity. The recent landmark Aged Care Work Value case has seen the Fair Work Commission grant a 15% wage increase for nurses and care workers in the sector as a “first step” towards securing better wages. Prime Minister Anthony Albanese has indicated that more stages would follow, including closing the gender pay gap.
The Secure Jobs, Better Pay Bill is critical in giving nurses and aged care workers access to a collective bargaining system that allows for wage growth increasing gender equity across
workplaces. The introduction of a statutory equal remuneration principle is also aimed to reduce barriers to pay equity claims.
The ANMF is advocating for greater flexibility in the workplace for nurses, midwives, and personal care workers, many of whom are women juggling multiple work and caring responsibilities.
“We want to see genuine access to flexible work arrangements. The threshold for employers to refuse a flexible working arrangement and the factors on which this is based, should be reviewed and recalibrated to a modern workforce. Our members report reducing their hours, moving to casual positions, or even resigning due to being denied flexible work arrangements,” said ANMF Federal Secretary Annie Butler.
“We want to see better opportunities to balance work with personal responsibilities – our working hours and workplace conditions were set in a very different domestic context to what we have today.”
This includes a reduction of ordinary working hours from 38 to 32 on the negotiating table.
There is a lack of national policy to redress the reduced earning capacity during a woman’s lifetime. Women continue to earn less than men do and are more likely to be engaged in casual and part-time work, which are also contributing factors to the gender gap in retirement savings. Many women are currently living their final years in poverty –with the next generation of women also at risk. Superannuation reforms have been welcomed including the removal of the $450 per month superannuation guarantee (SG) eligibility threshold. The SG rate will also increase from 10.5% to 12% by 2025.
The ANMF will advocate for further super reform, including mandatory superannuation requirements on all periods of parental leave, the introduction of a benchmark on retirement adequacy that doesn’t disadvantage women, and a fair share of super tax concessions for women.
Promisingly, supporting women’s workforce participation and advancing gender equality were highlighted in the Albanese Government’s first Budget. Several provisions were made for better-paid parental leave entitlements, access to childcare, paid family domestic violence leave, all which contribute to closing gender inequity.
Federal Labor has also committed to implement in full the recommendations of the Respect@Work report into sexual harassment in Australian workplaces. After years of tireless advocacy and campaigning by the ANMF, the ACTU and the broader union welcomed the introduction of 10-days paid FDV leave.
The ANMF in 2023 will continue to call for a national plan on gender equality.
FEATURE Jan–Mar 2023 Volume 27, No. 10 9
“We want to see better opportunities to balance work with personal responsibilities – our working hours and workplace conditions were set in a very different domestic context to what we have today.”
Improving equity in access to healthcare
Every Australian deserves access to quality and affordable healthcare, no matter who they are, or where they live. Yet, that’s not always the case.
The ANMF is calling for a range of measures to achieve health equity, including the review of health funding models, greater use of nurse-run clinics and nurse-led models of care, improving the capacity of the health system in rural and remote areas to meet community needs, and exploring digital telehealth opportunities, especially in rural and remote, and within nurse-led clinics.
According to ANMF Federal Secretary Annie Butler, a member of the Strengthening Medicare Taskforce, funding models should be reviewed so that they reflect the provision of healthcare, rather than activity, by providing incentives for outcomes such as improved health.
“The Taskforce is principally about improving primary healthcare,” Ms Butler explained.
“What we need to do in that space to ensure equal access for everybody and better outcomes for everybody.”
A key area of opportunity lies in giving nurse practitioners, and eligible midwives, expanded access to the Medicare Benefits Schedule (MBS) and removing barriers that prevent them from working to, and

extending and developing, their full scope of practice.
To achieve better integration between primary care, acute care, and aged care, Ms Butler says the ANMF is advocating for the expansion of models such as nurse-led clinics in primary healthcare, Queensland’s successful Nurse Navigators, and Canberra’s community-based nurse-led Walk-in Centres. Further, the ANMF would also like to see Urgent Care Centres, announced by the Labor Party, expanded beyond the first 50, and a commitment given to include nurse-led and multi-disciplinary options.
“The evidence consistently demonstrates that nurse-led models of care improve access to care, increase patient satisfaction and deliver better health outcomes,” Ms Butler said.
Advanced Practice Nurse Rachel Backhouse, who works across Canberra’s nurse-led Walk-in Centres, believes the communitybased model could be expanded nationally to improve access to healthcare.
Many patients access the centres because they are unable to see a GP, with one centre last year seeing 306 patients in a day, many
who would have otherwise presented to an Emergency Department and clogged up the hospital system.
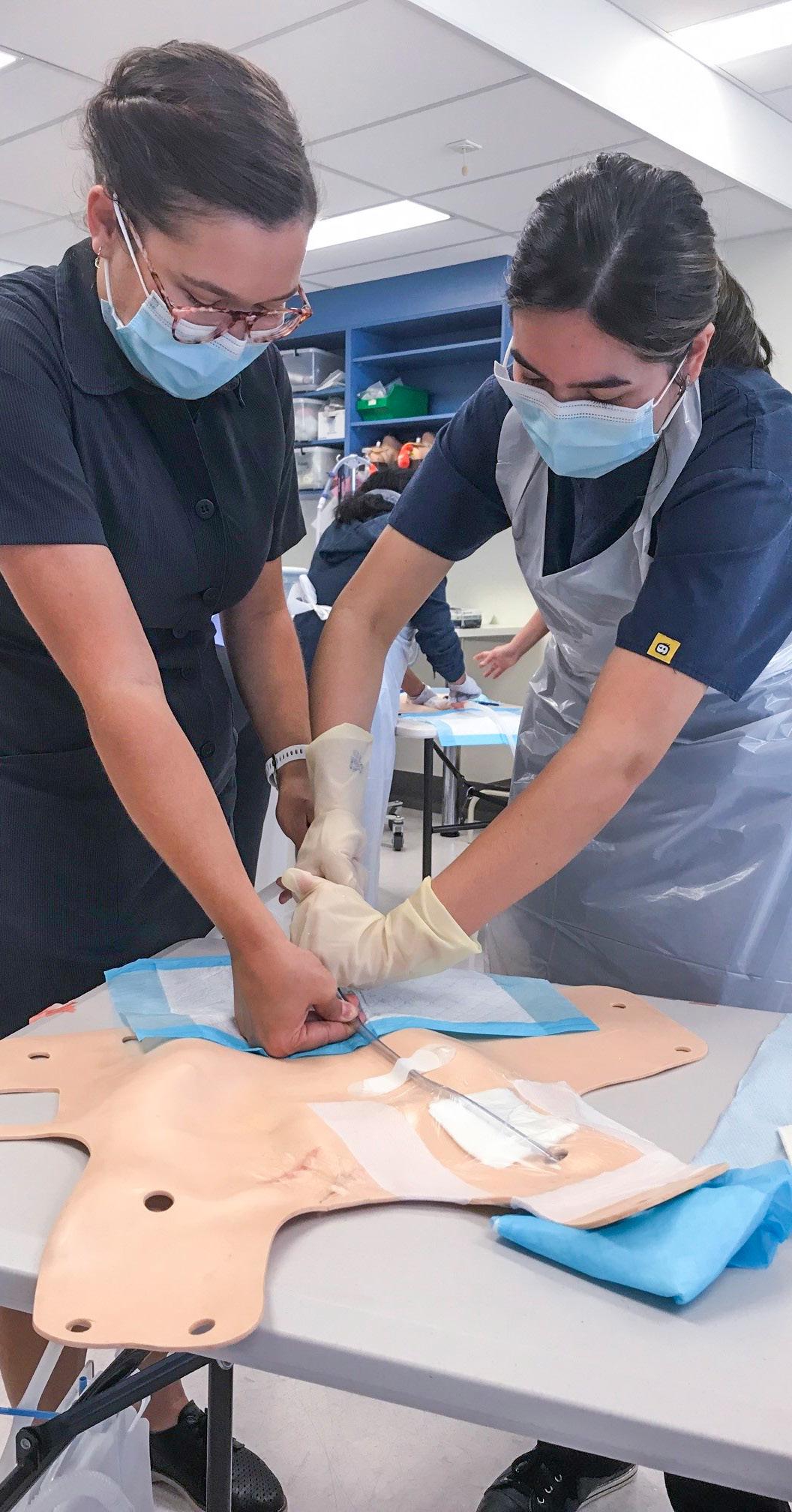
Nurses deliver care including ordering blood tests and X-Rays, and suturing. Nurse practitioners working in the clinics can also prescribe.
“We suture, we put casts on, we do a lot of things and we work with a lot of GPs as well. There’s a lot of work out there but we need to look at how we’re addressing primary healthcare in Australia because the emergency departments are just getting inundated with patients,” said Rachel, as part of a delegation of ANMF members who converged on Parliament House in Canberra last year to lobby politicians.
Extending and developing scope of practice for NPs will form one of the ANMF’s priorities in 2023.
Palliative Care Nurse Practitioner Juliane Samara, who works across 29 aged care facilities throughout the ACT, believes NPs can make a bigger difference in residential aged care and across the wider health system.
“We’re not a replacement workforce. We don’t replace doctors; we never want to replace doctors. We want to work as multidisciplinary teams. Nurses do that inherently and we do it well,” she said.
“The best models that I see are where everybody in the team is an equal member of that team. There’s no hierarchy but everybody knows what their role is and everybody knows that they can talk to each other, refer to each other and work together when there’s a need.”
FEATURE 10 Jan–Mar 2023 Volume 27, No. 10
“What we need to do in that space to ensure equal access for everybody and better outcomes for everybody.”
Aged care reform
After years of declining quality in care and neglect for elderly Australians, the Albanese Government acted on its election promises by commencing long-overdue aged care reform.
Landmark legislation, spearheaded by the Aged Care Amendment (Implementing Care Reform) Bill 2022, passed into law on 27 October 2022, will require aged care providers to have a registered nurse on site, and on duty, 24/7, from 1 July 2023. Aged care providers will also need to be more transparent and accountable regarding their use of taxpayer funding, including regularly publishing financial information on what they spend on care, nursing, food, maintenance, cleaning, and profits.

In its 2022-23 Budget last October, the Albanese Government, which labelled workforce its biggest priority, unveiled a $3.9 billion package of aged care reforms. They included a commitment to mandate the number of care minutes residents receive – beginning with 200 care minutes, including 40 from registered nurses, from 1 October 2023, and 215 care minutes, including 44 from RNs, from 1 October 2024.
ANMF Federal Secretary Annie Butler said the start of aged care reform offered renewed hope for members working in the sector.
“While implementation of these crucial reforms will take some time, ANMF members and aged care workers across the country will finally see the first real steps
towards actually fixing the aged care sector,” Ms Butler said.
“The implementation of a 24 hour RN presence and mandated minimum staffing laws will help address the chronic understaffing in the aged care sector.”
Other legislative improvements introduced last year included a Star Rating System to help older Australians compare residential aged care services; an enforceable Code of Conduct for aged care providers and workers; strengthening governance by placing new reporting requirements on providers; and extension of the Serious Incident Response Scheme (SIRS).
At Parliament House to witness passing of landmark RN 24/7 legislation, Palliative Care Nurse Practitioner Juliane Samara said having nurses around the clock in aged care was vital.
“People don’t stop dying and getting sick just because the roster finishes at 10 o’clock at night. They [residents] deserve and need registered nurses to be there to assess, treat and manage whatever symptoms they’ve got, around-the-clock,” she said.
“RN 24/7 will allow a range of facilities that function through a loophole in the system
at the moment to deliver a higher, safer, quality of care,” added NSW aged care RN Glen O’Driscoll.
Meanwhile, other budget measures included a new national registration scheme for personal care workers, costing $3.6 billion, home care administration and management fees capped and exit fees abolished, and a dedicated Aged Care Complaints Commissioner.
In 2023, another key priority for the ANMF will involve reducing public hospital admissions from aged care by increasing and embedding Residential In Reach (RIR) teams, including dementia specialists and nurses with psych-geriatric expertise, in public health services to meet local demand. The union also wants to expand the role of NPs in aged care, via a national plan.
More broadly, the ANMF is advocating for better career pathways into, and within, aged care. This includes funding transition programs that give early career nurses an opportunity to undertake post-graduate studies in gerontology, and supporting better skill mix and retention in the sector.
In a historic win, the ANMF’s aged care case for improved wages in the sector made inroads, with aged care workers securing an interim 15% pay rise after the Fair Work Commission (FWC) handed down its decision on the Work Value Case last November.
In summarising its decision, the FWC said the increase was “plainly justified by work value reasons”, supporting the ANMF’s claims that the work of aged care workers had never been properly valued and is in fact significantly undervalued.
FEATURE Jan–Mar 2023 Volume 27, No. 10 11
“While implementation of these crucial reforms will take some time, ANMF members and aged care workers across the country will finally see the first real steps towards actually fixing the aged care sector.”
Industrial relations reform
In late October, the Albanese Government took action to finally get wages moving, improve working conditions and achieve gender-equality across workplaces, with the introduction of its industrial relations legislation, the Secure Jobs, Better Pay Bill passed into law in December.
The Bill modernises Australia’s bargaining system, including better options for multi-employer bargaining rather than only enterprise bargaining. For example, unions could negotiate one pay deal across multiple employers in sectors such as aged care, with the more uniformed agreement shifting the power back to workers and increasing the ability to win fair pay rises.
“Our existing bargaining system is outdated and unfair and severely disadvantages workers in smaller, care industries – nurses and carers working in aged care simply have no power,” ANMF Federal Secretary Annie Butler said.

“Many of our members have been ‘lockedout’ under the existing bargaining system and haven’t had a proper wage rise in years,
with their conditions deteriorating to the point where more and more workers have abandoned their profession, leaving nursing homes dangerously understaffed.”
In Canberra to watch the Bill being introduced, NSW aged care registered nurse Glen O’Driscoll said it would help assist in recruiting and retaining staff.
“A casualised workforce has very little clout, very little security to tenure and very little benefits that a full-time employee gets. If this bargaining agreement can address those issues, that’s a plus, because it will assist retention in the industry and stop the exodus of skilled workers from our floor.”
Key focus areas the ANMF will lobby for industrial relations reform include creating
less burdensome threshold requirements for taking protected industrial action; advocating for permanent employment and only limited use of fixed term contracts; and keeping pressure on employers to comply with flexible working arrangement obligations rather than relying on casual work arrangements.
Importantly, the Secure Jobs, Better Pay Bill also introduced significant reforms to address the gender pay gap and discrimination.
The Fair Work Act will include an explicit prohibition on the sexual harassment of workers, prospective workers or a person conducting a business in connection with work. Meanwhile, the Fair Work Commission will be bolstered with two new expert panels, on pay equity, and the care and community sector, to help determine equal remuneration cases and certain award cases.
“This Bill is a step towards ending the wage crisis that working people have been battling through for a decade,”
ACTU Secretary Sally McManus said.
“This Bill will continue the work of making workplaces safer for women and making it easier for women to access and re-enter the workforce.”
FEATURE 12 Jan–Mar 2023 Volume 27, No. 10
“Our existing bargaining system is outdated and unfair and severely disadvantages workers in smaller, care industries – nurses and carers working in aged care simply have no power.”
Nursing, midwifery and care worker workforce
Globally there is a shortage of nurses and midwives. The pandemic has exacerbated health workforce shortages worldwide with many countries ill equipped and struggling to maintain adequate health service provision.
The Australian Department of Health forecast a national nursing shortage of about 85,000 nurses by 2025, growing to 123,000 nurses by 2030, in a detailed report on Australia’s future health workforce published back in 2014.

A broad range of factors influence the supply including the number of new graduates; the number of overseas nurses entering the Australian workforce; retention and workplace issues; and recruitment, along with the image of nursing.
For the past three years, nurses and midwives had been called to action like never before, ANMF Federal Secretary Annie Butler said.
“Many have reported feeling overwhelmed, anxious and exhausted. Anecdotally while many have left the profession altogether others have chosen to stay but have reduced their hours to cope.
“Lack of effective recruitment and retention of nurses and qualified care workers will only put further strain on a system at breaking point.”
A raft of recent measures including the Aged Care Bill, IR reforms, and flexible working arrangements may help to mitigate the exodus of those leaving the professions with better pay and improved conditions in sectors such as aged care. In addition, the government’s cost of living measures include for greater flexibility around paid parental leave and increased financial support for early childcare and education to support families.
The ANMF is working with government, alongside the Council of Deans of Nursing and Midwifery (Australia and New Zealand), the Nursing and Midwifery Board of Australia (NMBA), the Australian and Nursing Midwifery Accreditation Council (ANMAC) and other peak nursing bodies on strategies to grow our nursing, midwifery and care worker workforce and ensure a sustainable pipeline for the future. Proposed strategies include fully funded or subsidised undergraduate and postgraduate education and scholarships, reintroduction of HECS exemption, and an increase in the number of undergraduate places for both nursing and midwifery along with increased
funding and support for re-entry and return to practice programs.
“We need solutions to retain our current skilled workforce while we plan for how to recruit the next generation of nurses and midwives,” Ms Butler said.
Nurses and midwives have identified safe workloads, minimum staff ratios and skills mix, being paid overtime, wage increases and safe working conditions as key retention issues. Along with improved work satisfaction and being able to work to full scope of practice, in innovative models of care, and the ability to deliver high quality care.
The ANMF will continue to advocate for national ratios with federal health funding linked to minimum staffing requirements in all state and territory public health programs.
Mental health resources, adequate staff support and support programs for new nurses and midwives have also been highlighted as priority areas by members. The ANMF has welcomed the Albanese Government’s commitment to establish the National Nurse and Midwife Health Service which will provide health and wellbeing support for nurses and midwives across the country.
Supporting the development for a sustainable and experienced rural and remote workforce and greater efforts in our First Nations health workforce are also priorities for the ANMF in 2023.
FEATURE Jan–Mar 2023 Volume 27, No. 10 13
“Lack of effective recruitment and retention of nurses and qualified care workers will only put further strain on a system at breaking point.”
James Lloyd ANMF Federal Vice President

Student to RN – Our future
A successful student-to-graduate transition is critical in healthcare.
In this post-Covid world, healthcare workers, particularly nurses, midwives, and carers, are in high demand. But the last three pandemic years have resulted in a considerable increase in burnout, hence the need for a new workforce to be trained to meet this requirement. This new workforce will encounter immediate and extensive demands of an overstressed hospital system. So how can student RNs and midwives transition successfully to the workforce and lessen their chances of burnout and disillusionment?
Many years ago, at the start of my nursing career, I remembered the notion of “Eating our young”, coined by Judith Meissner in a 1986 article where she described the hostility new nurses faced at the hands of more experienced colleagues. The author even uses the term “a kind of a genocide” and “insidious cannibalism” to describe how we were treating our young (‘young’ meaning all new nurses and midwives, not an aged-based description) and its effect on our professions. This was a generation ago.
Nursing and midwifery were lifting slowly out of the ‘command and control’ system of the past. How we treated our young, denying their previous life experiences, skills they already earned, and taking initiative was frowned upon. Judith Meissner ended her article by stating, “If they are not nurtured as they develop, professional extinction beckons”.
Numerous studies have shown that limited support, unprofessional workplace behaviours, high workloads, and assigning responsibilities beyond their skills hamper the successful transition and integration of our student nurses and midwives. In a post-Covid world, there is a significant workforce shortage in nursing and midwifery professions. Our graduates transitioning to the workplace are being asked to work beyond their capacity. We are asking them to grow up quickly. The luxury of a smooth and steady transition from University/TAFE to the workplace is being truncated with the current demands.
Many students, prior to their graduate year, have external demands such as working to support themselves or having family responsibilities. These external stressors can result in decreased resilience before entering the new workplace. With external baggage, their early experiences in their graduate year will impact their level of satisfaction and could influence long-term career intentions.
What factors can influence a new graduate nurse’s transition into practice?
Teaching resilience – During the orientation of new graduates, resilience - a key ingredient of successmust be taught. Resilience is the ability to bounce back from adversity. It is a necessary skill for coping with life’s inevitable obstacles and one of the key
ingredients to any successful career. It is built by creating supportive work environments, developing a sense of belonging, having goals, celebrating successes, and having a good work-life balance. Building resilience in our graduates will ensure they have every chance of having a long and satisfying career in nursing or midwifery.
Creating a healthy work-life balance – A healthy work-life balance is crucial to a successful career. Generally, work has proven to be good for mental and physical health and wellbeing. But a poor work-life balance can cause stress and burnout. So as employers, mentors, and friends of new graduates, we need to encourage them to develop a rich and fulfilling life outside of work. This is a constant rebalancing act, and the equilibrium always shifts with life’s challenges.
Mentoring – Research indicates that effective mentoring is key to a graduate’s transition to the workplace. A good mentor must be objective and analytical and offer emotional support. A negative experience (for either the mentor or mentee) can have a detrimental effect on the relationship, such as suppressed student learning or the mentor unwilling to accept new students. The student-mentor bond is crucial to the new graduate’s successful transition and long-term stay in the profession.
Supporting emotional wellbeing – Finally, in my experience, the support of the emotional wellbeing of the new graduate is crucial. The new graduate needs to transition to a new workplace, develop new relationships, battle carer’s fatigue, cope with new stressors, work unfamiliar hours, and still take care of the emotional wellbeing of themselves and others (eg. family and partners) outside work. This convergence of competing stressors can challenge even those with a high emotional reserve. As mentors, role models and work colleagues, we need to look for the signs of burnout in our new grads. When seen, step in - open a conversation, ask if they need any help, listen, reassure, validate their feelings and concerns, encourage them to seek external professional help, and support without judgement.
This modern workplace can be a reality shock. Our new graduate nurses are entering a work environment characterised by nursing staff shortages, increasing patient acuity, Covid-19, and limited access to clinical support. A positive workplace environment makes a job more fulfilling and for a graduate, this is even more important, as it facilitates a more effective transition. In contrast, negative early experiences impact new graduate nurses’ satisfaction levels and can influence long-term career intentions.
Let’s empower our new graduates.
JAMES 14 Jan–Mar 2023 Volume 27, No. 10
Nurse & Midwife Support
o ers free, confidential and 24/7 health and wellbeing support to nurses, midwives and students across Australia.


Seeing the opportunity: Increasing the potential for eye donation
By Hayley M Hall and Sofia Karageorge
Corneal transplants can restore sight for people in the community, yet there is an imbalance in supply and demand.1 Worldwide, a staggering 12.7 million people are waiting on a corneal transplant. Annually, approximately 185,000 corneal transplants occur from 284,000 donated corneas; equating to only one in 70 transplants successfully received.1 In 2020, 2,277 Australians received corneal transplants from 1,318 donors.2
Palliative Care Units (PCU) inherently have a high death rate annually and staff often overlook these patients as potential eye donors.3 Palliative care patients in a ward-based setting are not suitable for solid organ donation; however, many patients are eligible to be eye donors.4,5 Facilitating the donation opportunity can fulfil a patient’s desire to help others in the community, acknowledge their registration status
on the Australian Organ Donor Register (AODR), their preferences outlined on their Advanced Care Directive and provide purpose for their families.4 Families who support eye donation can consent to whole eye or corneal donation. Whole eye donation includes the cornea, which restores sight and the sclera, which is used for surgical reconstruction in patients who have suffered from eye trauma or disease,
including glaucoma.2 Each eye tissue donor can potentially transform the lives of up to 10 people in the community.6

OVERVIEW
A quality improvement project was initiated in a 24-bed PCU in an outer-metropolitan 671-bed tertiary hospital. In 2017 the PCU had 553 deaths; however, only 11 eye donations occurred. While the hospital had two Donation Specialist Nursing Coordinators (DSNC) based in the Intensive Care Unit (ICU), eye donation was rarely considered for the PCU patients. Despite common misconceptions amongst healthcare professionals and the community, many patients who die in the PCU can donate their eyes.3 Whilst there are exclusion criteria, cancer and advanced age are not automatic exclusions.5 Corneal retrievals can occur up to 24 hours post death allowing staff adequate time to gain consent and alert the Lions Eye Donation Service (LEDS) with enough time for the one-hour retrieval process to occur.5
BACKGROUND
Exploration of eye donation was assumed to be standard practice for end-of-life care (EOLC) patients in the PCU; however, it was not initiated by staff. Despite having prepacked forms for completion by the bedside nurse when a patient died, including eye donation consent paperwork. There was no ward procedure for eye donation; instead,
16 Jan–Mar 2023 Volume 27, No. 10 CLINICAL UPDATE
it would predominantly occur if the family or patient raised the subject. A gap in this process was identified when a new nursing team member commenced on the PCU.
PROJECT OUTLINE
Two senior PCU nurses decided to reconsider the existing procedures. They became the Clinical Leads for eye donation in the palliative care setting. If a patient died in the ICU, staff would routinely refer to the DSNCs to check the AODR and screen the patients for organ, eye and tissue donation. While patients dying in the PCU would not be suitable for solid organ donation, many meet the criteria for eye donation.5,7 Unfortunately, a majority of potential inhospital donors are never considered for eye donation.8 Minimal donations occurred in the PCU as ward staff had limited knowledge about the eligibility criteria and the process of facilitating a donation. For eye donation to become a routine part of EOLC, education and support of the nursing staff are crucial.7
METHOD
Prior to the provision of education, the Clinical Leads sent out a survey to the PCU nursing staff to establish gaps in knowledge and attitudes to eye donation. The survey identified the following barriers to eye donation: a lack of knowledge regarding the donation process, misconceptions on eligibility and exclusion criteria, low confidence levels in conducting the donation conversation and
staff perception that raising eye donation with grieving families is inappropriate. Whilst the two Clinical Leads had basic knowledge surrounding the donation process. They set out to undertake further training and education to build knowledge and develop communication skills before implementing any new procedures.

The Clinical Leads sought education opportunities by connecting with DonateLife Victoria (DLV) staff based in the ICU and attending an education session and tour of the Lions Eye Donation Service (LEDS). DonateLife conducted formal training sessions, which the Clinical Leads attended. These included ‘Introductory Donation Awareness Training’ followed by ‘Core Family Donation Conversation’ workshop and ‘Practical Family Donation Conversation Workshop’.9 This knowledge enabled them to educate and up-skill ward staff, making the offering of eye donation standard practice on the ward.
The Clinical Leads conducted a staff inservice, which provided an overview of eye donation and addressed the perceived barriers from the survey. Given that the eye donation consent paperwork had been easily accessible and never used, the Clinical Leads implemented a new procedure to prompt staff to consider eye donation for every patient. With the information provided by LEDS 7 and guidance from the DLV staff, the Clinical Leads developed a screening tool to enable staff to
quickly determine a patient’s eligibility to donate their eyes and establish whether they were a registered donor. Nurses complete the screening tool for every patient on admission to the PCU. Once the goal of admission progresses to EOLC nurses request LEDS or DLV staff to conduct a register check. Donor register status was then reflected on the screening tool and the ward handover sheet. The screening tool was also valuable for highlighting a patient’s objection to organ and tissue donation. Patients’ organ and tissue donation preferences are often outlined in their Advance Care Directive or on the AODR.
The Clinical Leads provided 1:1 staff training to each nursing staff member. Topics covered include how to interpret and utilise the screening tool, identification of a registered donor and the timing and process of the donation conversation.
Instructions on completing the mandatory paperwork required for eye retrieval and donation to proceed were also part of the training. The staff survey also identified that most staff did not feel comfortable raising eye donation with families due to lack of experience and feeling it is insensitive to raise following a patient’s death.
Nurses were invited to observe donation conversations conducted by Clinical Leads to provide exposure to and alleviate any misconceptions around aggression or distress from families during these discussions. A key message taken from the DonateLife training
Jan–Mar 2023 Volume 27, No. 10 17 CLINICAL UPDATE
relayed to staff is that alerting families to the possibility of donation offers them an opportunity rather than trying to take something from them.9 At times, the LEDS conducted corneal retrievals on the ward, and nurses were encouraged to watch the procedure to eliminate any stigma attached to the retrieval process. Better understanding this empowered staff to confidently answer questions that patients or their families may ask. It also provided an opportunity for questions directed at the LEDS staff member undertaking the retrieval. Understanding how the corneal retrieval process works and the benefits experienced by the recipients enables staff to understand and support the process. The evidence suggests that explaining the benefits of corneal donation to the families of potential eye donors increased the consent rate and should be included in training.11
RESULTS
The initial focus of the quality improvement project in early 2018 included the Clinical Leads raising awareness of eye donation on the PCU via provision of education. The screening tool was implemented once there was basic knowledge around the eye donation process. Following the introduction of the screening tool and 1:1 education, there was a marked increase in the number of donation conversations occurring on the ward.
January – June 2018:
The Clinical Leads conducted ward inservices to raise awareness about donation and collected data on 206 patients who had died from 1 January 2018 to 30 June 2018. Half of these patients met the eligibility criteria
for eye donation. Out of 103 potential eye donors, staff approached nine families; two families declined, and seven consented to eye donation. Staff missed 91% of potential donors.
July – December 2018:
The Clinical Leads introduced the screening tool, and it was completed for every patient on admission. Clinical Leads collected data on the 351 patients who had died from 1 July 2018 to 31 December 2018. Of these, 128 patients met the eligibility criteria for eye donation. Fifty-one percent of potential eye donors were missed (40% reduction). Forty percent were offered eye donation by staff; 34 families declined and 28 consented to eye donation.
January – December 2019:
The screening tool was now a routine part of the ward admission procedure. All nursing staff had received 1:1 training from the Clinical Leads with an opportunity to observe or conduct a donation conversation. The Clinical Leads collected data on the 646 patients who had died between 1 January 2019 and 31 December 2019 and 183 met the eligibility criteria for eye donation. The screening tool reduced the missed potential donors to only 10%, 90% of those eligible were offered eye donation by staff; 81 families declined, and 83 families consented to eye donation.
2020 – 2021:
In 2020, there was a 13% decrease in eye donors nationally compared to 2019 due to service interruptions caused by the COVID-19 pandemic, which affected staffing levels and allowance of visitors on the ward.11,12
Despite the national trend, the PCU remained consistent throughout 2020 and 2021, with 88% of eligible patients offered eye donation in 2020, leading to 67 consents and 83% in 2021, resulting in 58 consents.
Over the lifespan of the project, 87% of identified registered donors consented to donation. The screening tool provided a place for nursing staff to document any comments made by the family when the donation conversation occurred. Of the recorded comments when a family declined, 19% stated it was because they “had never discussed donation with the patient”. Conversely, 24% had spoken with their relative and knew it was something they didn’t want. When raising via telephone, 52% consented.
Data was collected on 2,436 deaths since the beginning of the project. Of these 1,544, 60% were medically unsuitable. Of the 992 eligible patients, 212 (21%) were not
800 700 600 500 400 300 200 100 0 180 160 140 120 100 80 60 40 20 0 Deaths 2018 2019 2020 2021 Offered donation Missed potential donors 2018 2019 2020 2021 Eligible Offered donation PCU EYE DONATION STATS POST SCREENING TOOL AND STAFF 1:1 EDUCATION MISSED POTENTIAL DONORS VS DONATION OFFERED Missed potential donors Consented Declined CLINICAL UPDATE 18 Jan–Mar 2023 Volume 27, No. 10
offered donations due to the LEDS being unable to accept because of time constraints, excess supply, decreased capacity during holiday periods, and cancellation of elective surgeries during the COVID-19 pandemic.
DISCUSSION
Undoubtedly staff education and the implementation of the screening tool reduced the missed potential eye donors. The Clinical Leads considered the correct timing of the donation conversation and whether it was more ethical to speak about donation when the patient was still alive, providing the opportunity to be involved. As solid organ donation is extremely time sensitive, it is clinically imperative to conduct the donation conversation while the patient is alive, although acknowledging that in most situations, the patient would be unresponsive and unable to participate. The Clinical Leads agreed that admission to the PCU already brings big emotions for patients and their families. Nursing staff feared that raising the topic of donation pre-death could be considered pre-emptive and be ill-received. However, the choice of conversation timing is a limitation, as many families mentioned being unsure what their relative would want as a reason for declining donation. Knowing a patient’s status on the AODR can help families decide whether to support eye donation.13 Requesting donor register checks before raising eye donation with families was beneficial as families are made aware of any preferences expressed by the patient before they died. Periodically staff stated they could not raise eye donation at the time of the patient’s death for reasons such as relatives departing immediately or not attending the ward. Some families are exceptionally distressed, making it difficult to conduct any formal conversations. The Clinical Leads found that raising eye donation via a phone call to the senior available next of kin (SANOK) after death yielded positive consent rates. It is possible that when asked in person, relatives may have felt pressure to make an immediate decision. In contrast, a donation conversation via telephone allows for a decision to be made in a space they felt comfortable and receive it at a time when their emotions were less heightened.14
A common misconception highlighted in the staff survey was the belief that certain religions prohibited donation. Comments documented on the screening tool where families had declined eye donation, citing religious beliefs as the reason for declining, also reflected this misconception. As a result, a religious resource folder was compiled with statements of support for the donation process from heads of major religions, which were obtained from DonateLife resources.15 This was a useful tool for families who were conflicted on what the stance of the religion may be on donation.
LIMITATIONS
This was a single-site quality improvement project. While the program worked exceptionally well on this PCU, an identical model may not be suitable in other settings for reasons including the increased service demands and resourcing implications for the health service if there was a significant increase in donors.
While staff overlooked some potential donors due to human error, the most common reason documented for not raising donation was family aggression. Stressors created by the COVID-19 pandemic resulted in these incidences occurring more frequently.12,16
CONCLUSION
A simple change in practice has resulted in widespread benefits. Staff have described a sense of fulfilment gained by offering the donation opportunity to families during a sad time. We hope there are also benefits for the families involved who generously consented to eye donation. Educating staff to consider all patients for donation has resulted in a decrease in missed potential donors and an increased number of corneal donors and therefore transplants received by community members. To date 302 families from the PCU have consented to eye donation and have restored sight in approximately 503 recipients.
ACKNOWLEDGEMENTS
The authors thank the DSNCs based at Austin Health over the project’s lifespan for their overwhelming encouragement and guidance –Katheryn Hall, Ciara McGuigan, Sarah O’Connor, Clare Healy and Mikaela Henry. The LEDS staff who have always been generous with their knowledge – Dr Prema Finn, Adrienne Mackey, Gavin de Loree, and Prue Armstrong. They would also like to acknowledge the support of their Nurse Unit Manager, Hilary Hodgson and the PCU staff who have embraced this addition to the care they provide. Approval was obtained by the Austin Health ethics committee to evaluate this process. This research did not receive any funding. The authors declare no conflicts of interest.
AUTHORS
Hayley M Hall RN Grad Dip Palliative Care is an Associate Nurse Unit Manager on the Palliative Care Unit, Austin Health
Sofia Karageorge RN is an Associate Nurse Unit Manager on the Palliative Care Unit, Austin Health
REFERENCES
1. Gain P, Jullienne R, He Z, Aldossary M, Acquart S, Cognasse F, et al. Global Survey of Corneal Transplantation and Eye Banking. JAMA Ophthalmology. 2016 Feb 1;134(2):167.
2. Eye tissue donation: Why become an eye donor? | CERA [Internet]. cera.org.au. 2020 [cited 2022 Sep 27]. Available from: cera.org. au/lions-eye-donation-service/why-becomean-eye-donor/
3. Gillon S, Hurlow A, Rayment C, Zacharias H, Lennard R. Obstacles to corneal donation amongst hospice inpatients: A questionnaire survey of multi-disciplinary team member’s attitudes, knowledge, practice and experience. Palliative Medicine. 2011 9 September;26(7):939–46.
4. Eye and tissue donation awareness [Internet]. DonateLife. [cited 2022 Sep 24]. Available from: donatelife.gov.au/get-involved/eyeand-tissue-donation-awareness#Raisingawareness
5. Roach R, Broadbent AM. Eye Donation in Sydney Metropolitan Palliative Care Units. Journal of Palliative Medicine. 2010 Feb;13(2):121–3.
6. Williams L. Eye Donation Explained [Internet]. LifeSource. 2022 [cited 2022 Oct 1]. Available from: life-source.org/latest/eyedonation-explained
7. Identification and referral of eye donors [Internet]. [cited 2022 Sep 23]. Available from: cera.org.au/wp-content/uploads/2020/09/ Hospital-Referral-Flowsheet.pdf
8. Dutch MJ, Denahy AF. Distribution of potential eye and tissue donors within an Australian teaching hospital. Cell and Tissue Banking. 2017 11 December;19(3):323–31.
9. Professional training [Internet]. DonateLife. Available from: donatelife.gov.au/forhealthcare-workers/professional-training
10. Philpot SJ, Aranha S, Pilcher DV, Bailey M. Randomised, Double Blind, Controlled Trial of the Provision of Information about the Benefits of Organ Donation during a Family Donation Conversation. Herrero JI, editor. PLOS ONE [Internet]. 2016 Jun 20 [cited 2019 Dec 5];11(6):e0155778. Available from: ncbi.nlm.nih. gov/pmc/articles/PMC4913899/
11. 2020 Australian Donation and Transplantation Activity Report 2020 Australian Donation and Transplantation Activity Report [Internet]. [cited 2022 Sep 27]. Available from: donatelife.gov.au/sites/ default/files/2021-05/2020_australian_ donation_and_transplantation_activity_ report.pdf
12. Ahmed O, Brockmeier D, Lee K, Chapman WC, Doyle MB. Organ Donation during the Covid 19 pandemic. American Journal of Transplantation. 2020 13 July.
13. Rodrigue JR, Cornell DL, Krouse J, Howard RJ. Family initiated discussions about organ donation at the time of death. Clinical Transplantation. 2010 Jul;24(4):493–9.
14. Ting DSJ, Potts J, Jones M, Lawther T, Armitage WJ, Figueiredo FC. Impact of telephone consent and potential for eye donation in the UK: the Newcastle Eye Centre study. Eye (London, England) [Internet]. 2016 Mar 1 [cited 2020 Oct 29];30(3):342–8. Available from: https://pubmed.ncbi.nlm.nih.gov/26514245/
15. Community resource library [Internet]. DonateLife. Available from: donatelife.gov.au/ get-involved/community-resource-library
16. Heckemann B, Hahn S, Halfens RJG, Richter D, Schols JMGA. Patient and visitor aggression in health care: A survey exploring organisational safety culture and team efficacy. Journal of Nursing Management. 2019 29 May;27(5):1039–46.
CLINICAL UPDATE Jan–Mar 2023 Volume 27, No. 10 19
SAVE our planet PROTECT our health
THE CLIMATE CRISIS IS HERE. BUT THERE IS STILL TIME TO AVERT DISASTER IF WE TAKE ACTION NOW
The climate crisis predicted to happen sometime in the future has arrived. The fallout is evident, with poorer health, and wellbeing outcomes and environmental changes that sustains life. Science informs us if we continue along this trajectory, the impacts will get worse.
We can still mitigate climate change through sustainable practices which will reduce the burden on healthcare, and ensure a healthy plant.
Nurses and midwives, can be key players in change and make a significant difference by influencing the community to a more sustainable way of living.
The ANMJ wants to help all nurses and midwives achieve this goal for a sustainable future.
GLOBAL WARMING: HEALTH IS AT RISK BUT IS HEALTHCARE CONTRIBUTING TO THE PROBLEM?
Human-induced climate change is the most significant, most pervasive threat to the natural environment and societies the world has ever experienced, according to a report to the General Assembly in October last year. “The overall effect of inadequate actions to reduce greenhouse gas emissions is creating a human rights catastrophe, and the costs of these climate change related disasters are enormous,” says Ian Fry, Special Rapporteur on the promotion and protection of human rights in the context of climate change in the report.
To date, the planet has warmed more than 1.2°C compared with pre-industrial levels, resulting in profound and rapidly worsening health effects on every continent.1
IMPACT ON HEALTH AND HEALTHCARE
Planet warming is resulting in worsening health effects, health risks and the distribution of many infectious diseases. Heatwaves, for example, resulted in at least 350 deaths alone between 2000 and 2018 in Australia. As heatwaves increase in frequency and intensity more deaths are likely, with projected trends suggesting a potential increase of 10–50 additional heatwave days by the end of this century.2
Other extremes, such as fire, flood or drought, as well as high levels of pollution, can affect food security and access to supplies, including those necessary in healthcare.


Additionally, pollutants can be responsible for respiratory problems such as Chronic Obstructive Pulmonary Disease (COPD), asthma, bronchiolitis, lung cancer, cardiovascular events, central nervous system dysfunctions, and cutaneous diseases.1
WHAT IS GLOBAL WARMING
The United Nations, state global warming is caused by greenhouse gas emissions blanketing Earth. The gases trap the sun’s heat and holds it in the atmosphere, creating a greenhouse effect. As the world is warming faster than at any point in recorded history, warmer temperatures are changing weather patterns and disrupting the normal balance of nature over time.
20 Jan–Mar 2023 Volume 27, No. 10 ENVIRONMENT & HEALTHCARE
THE CAUSES
It’s widely known that electricity and heat production, agriculture, forestry, other land use, transportation and buildings are leading contributors through burning fossil fuels such as gas, petrol, oil, and coal to gases. Collectively they add an additional 9.1 billion tonnes of carbon to the air each year.3
Not so well known is that healthcare makes up 7% of Australia’s total emissions4 and globally 4.4% of emissions 5
Researchers say the most significant culprits of healthcare emissions are hospitals and the pharmaceutical industry, making up two-thirds of the carbon footprint.4 Ninety percent of the carbon footprint stems from indirect CO2 emissions due to purchases between multiple economic sectors that feed into the healthcare sector. The healthcare industry also produces millions of tonnes of waste, ending in landfills and adding to the carbon emissions in the atmosphere.3
As climate change progressively impacts the determinants of health, community and social structures, so too does the pressure on already burdened health services. As healthcare itself contributes to the collective carbon footprint, this sits at odds with the mission of healthcare professionals to increase the duration and quality of patients’ lives.4
Maiek et al.4 says for healthcare to reduce its carbon footprint there needs to be carbonefficient procedures, including greater public health measures, to lower the impact of healthcare services on the environment.
GOVERNMENT’S RESPONSE
Until recently, there had been little momentum on reducing healthcare emissions despite Australia’s peak Climate and Health Alliance (CAHA) strongly advocating for government action on sustainable healthcare. Since the Albanese Government took power in 2022, there have been promising signs of a shift.
According to CAHA, this includes the Government committing to Australia’s firstever national plan on climate and health and working towards sustainable healthcare with state and territory governments.
Additionally, Health Minister Mark Butler confirmed climate change as a health priority for the first time in the Australian Parliament. There are also moves to address our plastic pandemic.
CAN NURSES AND MIDWIVES INFLUENCE CHANGE?
“Absolutely,” says Ros Morgan, ANMF’s (Vic Branch) Environmental Health Officer. Ros argues it’s crucial nurses and midwives
work towards reducing the adverse health and environmental impact of climate change and the sustainability of the healthcare system.
“Taking action will improve healthcare delivery and generate cost savings,” says Ros.
Nurses and midwives represent a large proportion of the healthcare workforce and are positioned as spokespeople and advocates.
“We are trusted, visible and connected with community. Nurses and midwives can be effective bearers of the ethical story and immediate context of climate change impacts.”
As individuals, Ros says nurses and midwives can lead by example, reducing emissions in their personal and professional lives.
“The things that we do as individuals add up and can lead to changed expectation, demand and cultural shift. Ultimately, we can be part of system change.”
Ros stresses business as usual is not good enough as it gives us a trajectory well beyond what is liveable.
“Direct patient care is a valued part of our role, but we also contribute to best practice, quality improvement and system performance. We are the experts in our own area. We see the waste, the loss, and the opportunities. We are integral to consultative process and in delivering improved outcomes.”
*Read this story at anmj.org.au to view references

THE FACTS
Healthcare makes up 7% of Australia’s total emissions
Hospitals and the pharmaceutical industry make up twothirds of healthcare’s carbon footprint

90% of healthcare’s carbon footprint stems from indirect CO2 emissions from purchases between multiple economic sectors that feed into the sector.
The healthcare industry produces millions of tonnes of waste, ending in landfills and adding to the carbon emissions in the atmosphere.
NEXT ISSUE
Find out why hospitals and healthcare create green gas emissions and how you can be the change to save healthcare and the planet
Learn more and get involved
The Climate and Health Alliance are made up of 100+ health sector organisations and 200+ individuals leading action on climate to protect our health. They provide resources and advocacy on climate. caha.org.au
ANMF (Vic Branch) provide resources on their website. They also provide CPD and courses designed to strengthen advocacy and leadership around climate mitigation and environmentally sustainable workplace practice. The Branch runs an annual health and sustainability conference and has a green nurses and midwives facebook page that anyone can join. While information is directed to Victorian nurses and midwives, much of the content can be applied in other states and territories. For more information go to: anmfvic.asn.au/
HealthEnvironmentalSustainability
The Australian Commission on Safety and Quality in Healthcare has drafted a Sustainable Healthcare Module that is undergoing public consultation. Have your say what’s important to you. safetyandquality.gov.au/standards/ nsqhs-standards/sustainable-healthcare-module
& HEALTHCARE Jan–Mar 2023 Volume 27, No. 10 21
ENVIRONMENT
Sustainability in health champion
Meet OR nurse Sarina Henderson, a dedicated advocate for sustainable environmental practices at her work place at Melbourne’s St Vincent’s Hospital.
Sarina believes that nurses and midwives as healthcare professionals have a responsibility not only for the immediate care of their patients but also their future through protecting the planet of environmental impacts that affect health.
Sarina says one way nurses and midwives can do their bit is through recycling.
“Recycling can and does impact climate change by reducing the amounts going to landfill will therefore reduce emissions.”
Sarina has established a recycling bin in her staffroom, the collection of rigid plastic in the theatres and the collection of diathermy cables.
“Our recycling streams include paper, cardboard, rigid plastic, PVC, kimguard, aluminium, diathermy cables, batteries, polystyrene, and little blue towels (sterile cloth towels that come with sterile gowns to dry hands on).

“We also have a recycling bin in our staffroom and collect bottle lids, oral medication blister packs and stationery (pens and markers).”
Sarina says interest in sustainability in the department is spreading.
“There are now staff volunteering to help dispose of products at recycling collection points outside the workplace.”
She also has other staff members helping her with spreading the recycling message and finding ways to reduce and reuse supplies and equipment.
The team have come up with innovative ways to constantly remind staff to think about waste and the impact it has on the environment.
During national recycle week Sarina pulled together a reference guide on recycling streams, organised a pop quiz with prizes and had a recycling display with photos in their staff room.

Sarina’s advice to anyone wanting to introduce sustainable practices in their work place is to start small.
“Start something achievable. Pick one item or stream for recycling for example.”
Each issue we will be highlighting a sustainability in health champion. To nominate yourself or someone else, contact the ANMJ at ClimateActionForHealth @anmf.org.au
Every ACTION counts
Start small – Aim big Currently collecting plastic tops off IVAB vials. Weighing the PVC bags monthly before sending to recycling so that we can keep a track of amount recycled (only small ward – so only 1–2 kg per month at this stage). Aiming to educate to reduce disposable sats probe use.
Debra Roberts
Tearoom recycling
I reuse various plastic bags, I have a recycling bucket for aluminium pods in the tearoom, I pick up cans on way home from work.
Peter Veitch
Taking care of plastics
We keep the plastic V Wipes containers, I make the lid hole bigger and all small hard plastics get put in it. When full it goes into the hard plastics recycling bin.
Janeene Wolfe
Energy cuts
We minimise energy usage by cutting down fans, TV, heat exchange in rooms by proper closure and ventilation. Unplug beds, switch off lights, etc., in empty and unused rooms.
Jackie Sawyer
Sustainability tips
Share your sustainable practices at work and at home with the ANMJ so nurses and midwives nationwide can do their bit to save the climate. Together we will make a difference. One lucky contributor will also receive a $50 e-voucher from Koala Eco. Email ANMJ with your tip at: ClimateActionForHealth@ anmf.org.au
We don’t need to reinvent the wheeltofindwaystoreduceour impactontheplanet.
ENVIRONMENT & HEALTHCARE 22 Jan–Mar 2023 Volume 27, No. 10
Left to right: Sarina Henderson, Robyn Ingram, Amanda Luo , Zoe Butler
Linda Starr
An expert in the field of nursing and the law Associate Professor Linda Starr is in the School of Nursing and Midwifery at Flinders University in South Australia

Regulating cosmetic practice –a necessary reform in a growing industry
Cosmetic surgery and other cosmetic procedures have received considerable media attention in recent times – for the wrong reason.
This area of healthcare has blossomed into a billiondollar industry – tempting a number of registered and unregistered health practitioners to move into the sector. In the first instance, it is important to realise the distinction between cosmetic interventions and (reconstructive) plastic surgery – which is a specialty field that provides treatment for birth defects, diseases and injury.1
Cosmetic interventions, on the other hand, have historically been associated with the wealthy looking to retain or regain their youthful appearance and physique. However, today there is a broad range of individuals seeking cosmetic interventions that range from botox to liposuction, body part enlargements and reductions and the emerging practice of female genital cosmetic surgery such as designer laser vaginoplasty. Generally, these procedures are not medically indicated and often have little evidencebased guidelines for practitioners to follow. Each intervention, no matter how ‘minor’, is an invasive procedure and carries serious risks which must be conveyed to the consumer, which is an important component of the consent process and often missed in this area of practice.
• inappropriately sitting sedated patients up during surgery to comment on or consent to a breast implant;
• failing to provide adequate post-operative care for his patients;
• inviting friends and relatives to come into the operating room to obtain their opinion about a patient’s breast implants; and
• failing to keep appropriate records.
A further complaint related to the practitioner’s criminal conviction for conducting a private health facility without a licence - a contravention of the Private Health Facilities Act 2007 (NSW).2 The tribunal cancelled the practitioner’s license and issued a sevenyear ban from him, seeking a review of the decision.
References
1. Tansley P, Fleming D, Brown T. Cosmetic surgery regulation in Australia: Who is to be protected – surgeons or patients? The American Journal of Cosmetic Surgery 2022;39(3):161-165. doi. org/10.1177/07488068221105360
2. Health Care Complaints Commission v Blackstock (2020) NSWCATOD 110
3. See for example Medical Board of Australia v Dieu (Review and Regulation) (Corrected) (2014) VCAT 1597 a disciplinary case following the death of a young healthy woman following liposuction.
4. Access to the full report can be found at: kwm.com/au/ en/insights/latest-thinking/ release-of-independentreview-into-cosmeticservices-industry.html
5. nursingmidwiferyboard. gov.au/codes-guidelinesstatements/positionstatements/nurses-andcosmetic-procedures.aspx
6. medicalboard.gov.au/codesguidelines-policies.aspx
Whilst there are some very skilled and competent practitioners working in this field, there is also a small number who have embarked on this career path despite not holding any relevant qualifications and with various levels of competency. Currently, in Australia any medically qualified practitioner can perform these procedures and use the title cosmetic surgeon without holding formal qualifications. The only accredited medical professionals recognised by Ahpra to perform reconstructive and cosmetic surgery are plastic surgeons.
There have been a number of disciplinary proceedings against practitioners working in this sector where accepted standards of practice have not been met, including the post-operative care phase.
In 2020 Dr Blackstock was found guilty of unsatisfactory professional conduct and professional misconduct after providing cosmetic surgery to 11 patients. The complaints included:
• A failure to conduct appropriate pre-operative assessments of patients and to obtain proper informed consent from them;
The exposure of the serious harm that some patients have endured as a result of some cosmetic procedures has revealed a mostly unregulated area of practice in need of serious rapid reform.3 In 2021, both Ahpra and the Medical Board of Australia called for an independent review of this sector, resulting in 16 recommendations being made to address a range of issues. All have been accepted by both Ahpra and the MBA,4 who are working together to provide consumers with greater protection from poor practice and unqualified practitioners in this sector.
The Nursing and Midwifery Board of Australia has published a position statement for nurses working in cosmetic medical procedures.5 It is important that those working in this field are familiar with this document and also the MBA’s6 guidelines for medical officers performing cosmetic medical and surgical procedures to ensure they are practising in accordance with the expected level of competency and within their scope of practice.
Whilst the disciplinary proceedings, in this case, focused on the medical officer, this practitioner did not work alone. All health practitioners have an important role as a patient advocate and have a professional responsibility to take appropriate action where they hold a reasonable belief that another health practitioner is acting inappropriately or not meeting reasonable practice standards and putting patients at risk of harm. These cases are an important reminder of the need to fulfil this role rather than assume the role of a silent witness.
LEGAL Jan–Mar 2023 Volume 27, No. 10 23
The dilemma: International recruitment of nurses and midwives amid a global workforce shortage
 By Natalie Dragon
By Natalie Dragon
24 Jan–Mar 2023 Volume 27, No. 10
Historic chronic underinvestment of nursing and midwifery, compounded by a global pandemic, has left a perilous shortage of the world’s largest health workforce.
The COVID-19 pandemic has worsened the already fragile state of the global nursing workforce, with the estimated global shortage of nurses and midwives at 30.6 million.
“Essentially the demand for nurses has outstripped supply. Many countries were experiencing shortages of nurses before COVID-19. The pandemic has further exposed these existing staffing gaps”, Adjunct Professor, WHO Collaborating Centre, University of Technology, Sydney, James Buchan told the ANMJ.
“It’s the great resignation – more nurses are retiring early, or working fewer hours or are moving to less demanding work –which is increasing the gap between supply and demand. On the back of that higherincome countries in the OECD are engaging in active international recruitment of other countries.
“What we are seeing is a chase for talent and there’s not enough to go around.”
The World Health Organization (WHO) has declared active recruitment of healthcare workers from less-resourced countries to meet the healthcare needs of well-resourced nations and its related migration as one of the greatest global threats in the 21ST century.
Emigration rates for native-born nurses exceed 50% in 20 countries, which are mainly small islands in the Caribbean and the Pacific, according to the Organisation of Economic Co-operation and Development (OECD).
“There are Pacific Island countries where there are very small numbers of nurses and who are very vulnerable, even losing 10-20 nurses can have a significant impact on their health system,” Professor Buchan said.
According to the ICN report COVID-19 and the international supply of nurses, 550,000 foreign trained nurses are working across the 36 high-income OECD member countries (up from 460,000 in 2011). This includes 197,000 nurses in USA, 100,000 in the UK, 71,000 in Germany, and 53,000 in Australia.
“In the UK, recruiting nursing numbers is the highest it’s ever been since 1990 when we started collating the data. The NHS had 38,000 nurse vacancies before COVID which has grown to 45,000 – 10% or one in 10 RN vacancies in the NHS,” Professor Buchan said.
In June 2022, the Royal College of Nurses, UK, reported a ten-fold increase in nurse recruitment from ‘red list’ countries - those identified as having serious workforce challenges that must not be targeted for active recruitment. For example, 3,000 nurses from Nigeria, a red-list country, were registered in the UK last year.
The WHO Code of Practice framework on ethical recruitment, endorsed by all member states, outlines that high-income countries do not engage in large scale active recruitment of low-income countries. However the Code is voluntary and the definition of ‘active’ is not clearly defined. In addition, the code was set out in 2010 before recruitment via social media.
“Country A may send out a message via social media that there are vacancies, and doesn’t target any country, so this is ‘not active’. It’s a very grey area,” Professor Buchan said.
At the May 2022 World Health Assembly, the ICN pleaded for governments to comply with the WHO Code of Practice and invest in nursing education with the aim of greater self-sufficiency in the supply of nurses.
ICN Chief Executive Officer Howard Catton said governments must address their own shortages by increasing the number of home-educated nurses and investing in retaining their current nurse workforce.
“It comes back to underinvestment in the nursing profession,” says Catton. “It is crucial that all countries train and retain more of their own nurses and implement ethical recruitment practices when they employ nurses from overseas.
“Career mobility is important for many nurses: it enables them to further their professional development, maximise their skills and qualifications, and fulfil their personal career goals.

“But there have been many cases of internationally educated nurses being poorly treated by their employers, and some countries that can ill-afford to lose their nurses have been left with insufficient numbers because of aggressive recruitment from overseas.”
The ICN calls on governments and employers to adopt appropriate policies when taking nurses from other countries.
Professor Buchan concurs. “It’s only fair those nurses have full information about the job they are coming to, the pay rates, and access to continuing development opportunities.
“It’s not something [recruitment] that ends the day the nurse gets off the plane. Careful consideration needs to be given to their settlement in the country, including what may be an unfamiliar culture, climate, and so on.”
In Australia, international recruitment has been a strategy regularly used to resolve workforce shortages. More recently, the government has been looking at lifting Australia’s skilled migrant cap by 35,000 per year up to 195,000.
ANMF’s policy on International recruitment of nurses and midwives clearly outlines that overseas recruitment must not be the primary strategy to overcome nursing and midwifery shortages in Australia.
“Governments must commit more resources for workforce planning, education and improving pay and conditions in order to attract and retain domestic nurses and midwives,” ANMF Federal Secretary Annie Butler said.
Policies should be adopted, both at country and international levels, to ensure nurse supply, says Professor Buchan. This includes by assessing and improving nurse workforce data, reviewing and expanding the capacity of the domestic nurse education system, assessing and improving retention of nurses and the attractiveness of nursing as a career, implementing policies to optimise the nursing workforce contribution, and monitoring and tracking nurse self-sufficiency.
“In the UK what is emerging is there is a high level of turnover of nurses in their 20s and early 30s not just pre-retirement in their 50s. We need to understand what is motivating them to leave.
“Safe staffing, workload, wellbeing, access to flexible hours and the ability to reduce their hours are at the core. We also need to ensure pay rates keep up with the cost of living,” Professor Buchan said.
“Pay and career structure that recognises and rewards nurses in advanced practice roles and nurse practitioners is also key. One of the problems is that nurses cannot scale up the career pathway. Many systems are under cost containment pressures with governments avoiding pay rises.”
In addition, workforce policies need to improve working conditions for women and to close gender gaps in leadership and pay, said Professor Buchan.
INTERNATIONAL Jan–Mar 2023 Volume 27, No. 10 25
By Dr Megan-Jane Johnstone AO
Retired Professor of Nursing and Independent Scholar
The call for morally just global action
The COVID-19 pandemic together with other global pressures that have been placed on the world’s healthcare systems have converged to highlight the prediction – and now reality – of a catastrophic shortage of nurses.

References
1. International Council of Nurses (ICN). The global nursing shortage and retention. 2021. Available from: icn.ch/system/ files/2021-07/ICN%20
Policy%20Brief_Nurse%20 Shortage%20and%20 Retention.pdf
2. Ferguson SL, Trent-Adams S, Tlou S. A Call to Action: Let’s Implement and Evaluate the WHO’s Strategic Directions for Nursing and Midwifery Right Now. Nursing Economic$; 2022: 40(4)
3. Peters M. Time to solve persistent, pernicious, and widespread nursing workforce shortages. (Under review)
4. Adler RP, Goggin J. What do we mean by “civic engagement”? Journal of Transformative Education 2005; 3(3):236-53
As the world grapples with how to remedy the erosion of the nursing workforce and build its sustainable future, leaders have been giving prioritised attention to the issues of how best to retain nurses educated domestically and how best to attract future candidates into the profession in both the short and long term. Their attempts are (and will continue to be) fraught, however, as demand exceeds supply in the present, and the education and retention of future generations of nurses takes time. In an attempt to overcome this problem, high-income countries have engaged in the ethically questionable practice of seeking to augment their nursing workforce by ‘increasing their reliance on international nursing recruitment’.1(P4) This practice is ethically questionable because it stands perilously close to ‘poaching’ nurses from countries who can least afford to lose their existing establishments of equivalent full-time nursing staff.
In a recent article calling for ‘less talk and more action’, Ferguson and colleagues2(P187) correctly argue that ‘every country needs to hit the reset button and each of us need to do our part’. They go on to argue that what is particularly needed is a ‘broad coalition’ of whoever (eg. from a range of sectors including health, education, security, environmental, agricultural) and whatever it takes to bring about change, otherwise things will go backwards.2(P187)
The conundrum surrounding the global nursing shortage is not new. Neither are the well documented strategies for addressing it: enhancing workforce retention, improving recruitment, encouraging and enabling a return to practice and, where ethical, international recruitment.3 One strategy that has yet to be recognised and explored, however, is civic engagement – a strategy exemplified by the political manoeuvrings of Florence Nightingale and her legendary influence on reforming the quality and safety of healthcare in the 19TH and 20TH centuries.
Civic engagement may be defined as ‘the ways in which citizens participate in the life of a community in order to improve conditions for others or to help the community’s future’.4(P236) In the protracted aftermath of COVID-19, citizens are being granted a unique opportunity to reflect on and consider what they want and can reasonably expect of nurses and a nursing workforce, and what sacrifices they are prepared to make in order to ensure that when the situation arises, the nursing services they want, need and expect will be available.
Nursing by its very nature is of high value. Nursing matters. Nurses matter.
Nurses matter because the work they do is significant. Their work is significant because it makes the lives of others significant – it gives value to the lives of others by treating them as being worthy of attention and care. During the COVID-19 pandemic, nurses repeatedly went above and beyond the call of duty. Now it is time for the world’s leaders and health authorities to likewise go above and beyond, and to fully engage in the conscientious action that is so desperately needed to redress the status quo.
The full version of this extract is available in issue 39(4) of the Australian Journal of Advanced Nursing Johnston M-J. Nursing shortages and the ‘Tragedy of the Commons’: the demand for a morally just global response. Aust J Adv Nurs. 39(4):1-3. Available from: doi.org/10.37464/2020.394.1024
INTERNATIONAL 26 Jan–Mar 2023 Volume 27, No. 10

Organised by the International Council of Nurses NURSES TOGETHER: A FORCE FOR GLOBAL HEALTH REGISTER NOW! In partnership with the Canadian Nurses Association #ICN Congress #ICN2023 @ICN urses
The ANMF National Policy Research Unit – the first five years
By Casey Marnie and Micah DJ Peters

Embedding high-quality research into nursing and midwifery is vital for delivering safe, effective healthcare.
This is not only important in informing best practice, but having the latest evidence is essential to the ANMF as they advocate for the rights of the nursing and midwifery workforce and support improvement to the health and wellbeing of all community members.
To grow the research capacity of the ANMF and, in turn, to enhance and embed research into nursing and midwifery more broadly, in 2018, the National Policy Research Unit (NPRU) of the ANMF Federal Office was established in partnership with the University of South Australia’s Rosemary Bryant AO Research Centre.
As we approach the end of the 5TH year since inception of the NPRU, we reflect on the work we have undertaken, the ANMF’s achievements, and future opportunities for how the Unit can continue to best support nurses and midwives.
In concordance with the priorities of the ANMF at a federal level, we have led significant bodies
of work across a range of issues. Ongoing and Australia-wide focus on aged care has seen us make many contributions to submissions to the Royal Commission into Aged Care Quality and Safety.
In doing so, all submissions have included evidence drawn from published literature, including our own.1-8 Subsequent work in aged care, following on from the release of the Royal Commission’s Final Report has contributed to the aged care campaigns of the ANMF leading into the 2022 election and in the momentous legislation of mandatory staffing levels in residential aged care facilities including 24/7 registered nurse presence and wage increases for staff.
Another focus of the unit has, of course, been COVID-19. As the pandemic evolved, our priority has been to ensure that nurses and midwives are provided with up-to-date, accurate, and reliable information to inform decision-making at all levels.
We have published many evidence briefs on COVID-19 and variants, personal protective equipment, and contemporary information regarding vaccines and vaccination strategies.9–12
Importantly, the voices of members have been critical with responses to national surveys of Australia’s nursing, midwifery, and personal carer workforce underpinning national reports that highlight the struggles that nurses and midwives face as the pandemic evolves.8,12
We have also provided regular comprehensive updates to the ANMF leadership on the state of COVID-19 around the nation.
These updates ensure the state of COVID-19 is clear and interpretable as the ANMF advocates for the conditions of staff on the ground.
Another primary function of the Unit is, in collaboration with branches, oversight of the national research program of the ANMF via the national Research Strategy and Advisory Committee.
RESEARCH 28 Jan–Mar 2023 Volume 27, No. 10
Micah DJ Peters (left) and Casey Marnie (right)
References
1. Peters MDJ, Marnie C, Butler A. Delivering, funding, and rating safe staffing levels and skills mix in aged care. International Journal of Nursing Studies. 2021;119(103943).
2. Peters MDJ, Marnie C. Human costs of aged care productivity: innovation versus staffing and skills mix. Collegian 2021; 28(3):351-355.
As
we approach the end of the 5TH year since inception of the NPRU, we reflect on the work we have undertaken, the ANMF’s achievements, and future opportunities for how the Unit can continue to best support nurses and midwives.
We facilitate collaborative relationships with national and international research centres and inform ANMF participation in research aligned to the needs and interests of ANMF members.


This function of scholarly engagement is also embedded in our editorial work and stewardship of the ANMF’s Australian Journal of Advanced Nursing. Here, we seek to promote a wide variety of original research and scholarly work to inform and empower nurses and midwives to deliver evidencebased practice.
Located within a university, we also support nurses and midwives to develop research capacity, providing supervisory support at the PhD and Masters levels.
Further, through a vacation scholarship opportunity for UniSA undergraduates, we have developed a program to support research engagement for undergraduates seeking to build research skills and confidence.
Early exposure to research supports nurses and midwives to pursue future research opportunities and has greater influence in clinical environments.
Over the coming years, we will use our diverse and multi-disciplinary expertise to lead and collaborate on a variety of research projects focussing on key topics from the aged care workforce and nurse practitioner models of care to cancer nursing, climate change impact, workforce policy, and First Nations health and wellbeing.
While this brief column can’t cover all the work we’ve achieved over the last five years, we hope to continue working with the ANMF and its members to strengthen the contribution of nursing and midwifery to improving Australia’s health and aged care systems and the health of our national and global communities.
Authors
Casey Marnie BCom(econ) and Micah DJ Peters PhD work at the National Policy Research Unit (Federal Office), Australian Nursing and Midwifery Federation (ANMF) and the University of South Australia, Clinical and Health Sciences, Rosemary Bryant AO Research Centre.
3. Bonner R, Peters MDJ, Butler A. Workforce – the bedrock of aged care reform. Australian Economic Review. 2021;54(2):285-293.
4. Peters MDJ, Marnie C, Butler A. Royal Commission into aged care recommendations on minimum staff time standard for nursing homes. Australian Health Review 2022;46(4):388-390.
5. Peters MDJ, Marnie C, Butler A. Putting people first: the importance of recommending minimum staffing levels and skills mix. Journal of Law and Medicine. 2022;29(2):380387.
6. Peters MDJ, Marnie C, Butler A. ANMF National Aged Care Survey 2019 – Final Report. ANMF: Online. 2019.
7. Peters MDJ, Marnie C, Butler A. National aged care survey 2019 – community member companion report. ANMF: Online. 2019.
8. Peters MDJ, Marnie C. National Aged Care COVID-19 Survey 2022 Final Report. ANMF: Online. 2022.
9. Peters MDJ. Addressing vaccine hesitancy and resistance for COVID-19 vaccines, International Journal of Nursing Studies 2022;131(104241):1-16.
10. Peters MDJ, Marnie C, Butler A. Policies and procedures for personal protective equipment: does inconsistency increase risk of contamination and infection? International Journal of Nursing Studies. 2020;109(103653):1-4.
11. Peters MDJ. N95 respirators for healthcare workers: the importance of fit, comfort, and usability. Medical Journal of Australia. 2022;217(2):83-84.
RESEARCH Jan–Mar 2023 Volume 27, No. 10 29
is the official peer-reviewed journal of the ANMF and is dedicated to publishing and showcasing scholarly material relevant to nursing and midwifery professional, clinical, research, education, management and policy audiences.
12. Peters MDJ, Marnie C. Australian Nursing and Midwifery Federation National COVID-19 Survey 2022Public and Private Hospitals. ANMF: the publication on the AJAN website: ajan.com.au
AJAN
Access
The perfect place to work
Julianne Bryce ANMF Federal Senior Professional Officer

Trouble parking, reallocation, re-deployment, short staffing, colleagues off sick, lack of support, poor communication, no recognition, and not feeling safe – just to name a few. If issues remain unresolved, we then have to decide whether to stay or look for work elsewhere.
The recruitment and retention of nurses and midwives is a global issue. Nursing and midwifery shortages are being experienced worldwide. This global shortage further contributes to nurses and midwives being overworked and dissatisfied. The provision of care also suffers.1
Nursing ethics expert Dr Megan-Jane Johnstone AO calls this the ‘tragedy of nursing’ and equates this to the ‘tragedy of the commons’. The tragedy of the commons, an economic theory first proposed in 1833, occurs when ‘individuals with access to a public resource (also called a common) act in their own interest and, in doing so, ultimately deplete the resource’.2 In this case, the shared resource of healthcare provided by nurses and midwives will be impacted by their need to act in their own self-interest to leave the professions if the issues they face can’t be resolved.3
Recently some of my colleagues have been confronted by constant, relentless re-deployment. Management has continued to recruit to their ward despite this daily occurrence of their staff being sent elsewhere. Although re-deployment is always a possibility, when it happens every day, this takes a personal and professional toll. When you apply to work on a particular ward, isn’t it reasonable to expect that you will mostly work there and not constantly be sent elsewhere?
A positive practice environment requires strong nursing and midwifery leadership, an inclusive management style, autonomy for nurses and midwives, positive relationships with colleagues, good resources, quality career development, continuing professional development and further training, and good prospects for promotion.
Key characteristics of quality workplaces include good management practices, professional recognition, support structures, education and work health and safety.
References
1. World Health Organization. Nursing and Midwifery Fact Sheet. 2022. Available at who.int/news-room/factsheets/detail/nursing-andmidwifery
2. Harvard Business School Online. Tragedy of the commons: What it is and 5 examples. 2022. Available at: online.hbs.edu/blog/post/ tragedy-of-the-commonsimpact-on-sustainabilityissues
3. Johnstone MJ. Bioethics: A nursing perspective. 8TH edition. Melbourne. Australia 2022.
4. International Council of Nurses. Positive practice environment Fact Sheet. Geneva. Switzerland. 2007
5. Queensland Nurses and Midwives’ Union. Positive practice environment standards for nursing and midwifery. QNMU Office. 2020. Available at: qnmu.org.au/web/ campaigns/ppe-standards. aspx
The systemic problems of workload and the lack of a positive practice environment are major contributors to nurses’ and midwives’ stress, burnout and fatigue. Workload should be addressed using mandated, legislated, evidence-based ratios. Of course, nurses and midwives should be paid more but not just in bonuses. This should be in the form of real wage reform in enterprise agreements. Although we all go to work to be paid, money isn’t the sole motivating factor in nurses’ and midwives’ decisions to stay or leave. We know this from past experience negotiating agreements and arguing for safe staffing and safe workplaces.
Now, more than ever, establishing positive practice environments is essential to attracting, motivating and retaining staff. In the face of challenges presented by the COVID-19 pandemic, how can we create and maintain a positive practice environment? What does it even look like?
Positive practice environments are settings that support excellence and decent work. In particular, they strive to ensure the health, safety and personal wellbeing of staff, support safe, quality person-centred care and improve the motivation, productivity and performance of individuals and organisations.4
Mutual respect, consideration and constant communication are basic components of workplace culture that must be established and rigorously maintained.
Over the years, nurses and midwives have endeavoured to define and create positive practice environments. Recent work by the ANMF Queensland Branch (QNMU) is a great example.
The QNMU has developed Positive Practice Environment Standards for collaboration, autonomy and safety. These Standards detail that, for optimum health outcomes, nurses and midwives need:
• Safe staffing levels;
• Physical, psychological and cultural safety;
• Autonomous and collaborative practice;
• Shared governance and decision-making;
• Research and innovation; and
• Transformational leadership.5
Together, these five elements are the Positive Practice Environment Standards.
How well is your workplace doing in these areas?
Workplaces incorporating these Standards into their strategic direction can avert the ‘tragedy of nursing’, improve nurses’ and midwives’ wellbeing, mitigate burnout, and positively impact nurses’ and midwives’ satisfaction and retention.
What makes a great workplace? Do we know what to look for when choosing a place to work? It’s often the case that we very quickly recognise what we don’t want in our workplace when confronted with it every day.
PROFESSIONAL 30 Jan–Mar 2023 Volume 27, No. 10
Nurse Practitioner
Lesley Salem’s passion for Aboriginal health
Robert Fedele
Improving the health and welfare of Aboriginal people has always been front and centre for nurse practitioner Lesley Salem.
checks and still need to wait for a doctor to turn up and sign their approval.
“The majority of people providing care in that area are nurse practitioners. We need to be able to do the things that these communities need us to, like Close the Gap initiatives to provide total care for these people.”
During her career, Lesley has worked across many diverse settings including hospitals, a detention centre, and Aboriginal Community Controlled Health Services.
Nearly 20 years ago, Lesley became the first Aboriginal person to be endorsed as a nurse practitioner in Australia. It still ranks among her greatest achievements.

Yet, at the time, Lesley kept her Aboriginality hidden because she wanted to earn the title on merit, not simply to meet a quota.
Significantly, Lesley has continued to be a strong advocate against racism across the health system and society throughout her nursing career. Regrettably, there is still a long way to go.
She is currently taking part in a coroner’s inquest examining accusation of racism at the local hospital.
“It [racism] is very much alive and well,” she says.
However, Lesley remains confident that as more First Nations nurses and midwives enter the health system real change can occur in the health and welfare of Aboriginal and Torres Strait Islander people.
“They’ve got a heavy burden on their shoulders,” she says of early career Indigenous nurses.
A fly-in fly-out remote area nurse, Lesley currently works as a generalist and chronic disease NP in Doomadgee, a remote Aboriginal community in far north-west Queensland, as well as nearby Mornington Island.
Her scope of care includes assessing clients, performing diagnostic examinations and tests, and treating and managing them. She also runs a skin clinic at the local school, care at the aged care facility, daily clinics, and care at health promotion days.
In June last year, she was awarded the Member of the Order of Australia (AM) in the 2022 Queen’s Birthday Honours List for significant service to nursing and to Indigenous health.
She describes feeling humbled by the honour, largely because it was her peers who nominated her.
“I’m really grateful for the award and what it’s for because I’ve been trying to get in to see influential people who can help change things up the scale. My dad always said any award you get it’s like giving you a free soapbox in front of the people that matter. All I want to do is use this to open doors with this new government to allow me to say the things I think need doing.”
In remote towns like Doomadgee, Lesley says there is urgent need for more nurses and nurse practitioners to deliver healthcare. Part of the problem is barriers to access. For example, nurses conduct health
“My generation failed to Close the Gap, and try as we might, we still haven’t achieved it. There’s a huge amount on the shoulders of our next generation of nurses and they will be brilliant. They’ve been taught and better prepared and I feel absolutely assured that they will take on the burden more so than we’ve been able to take it on and I’m sure they’ll Close the Gap in life disparity for Aboriginal people.”
WORKING LIFE Jan–Mar 2023 Volume 27, No. 10 31
(left) Lesley Salem
A clinical pathway for management of dementia related behaviours in residential aged care facilities
 By
By
32 Jan–Mar 2023 Volume 27, No. 10 CLINICAL REVIEW
Kate Kennedy, Deborah Forsythe, Joanne Wagner, Greg Sharplin and Marion Eckert
In 2022 approximately 500,000 people were living with dementia in Australia, and around 1.6 million people were involved in their care. About 90% of people living with dementia will experience changed behaviours.1
The Rosemary Bryant AO Research Centre was approached by an Eldercare site manager to help ensure they were providing the best quality dementia care, based on current best practice evidence, that met current and new quality care requirements.
Together, we decided a clinical pathway for use by staff to prevent, delay or manage the onset of changed behaviours could help reduce dementia specific Emergency Department visits, specialist referrals, quality of life and antipsychotic medication use.
Clinical pathways provide structured plans that improve quality of care, reduce variation and maximise treatment or health outcomes in a specific group.2 Use of one could also provide a structured record trail of processes for auditing or quality purposes. Our aim was to improve clinical outcomes and quality of life for people with dementia with a pathway that was practical, acceptable, and could be integrated into current site processes.
METHODS
A rapid, systematic review of the literature was conducted to find an existing clinical pathway for managing changed behaviours in RACFs by nurses.3 No relevant pathway was found, so a draft pathway was developed based on clinical practice guidelines found in the literature.4 A multidisciplinary team of researchers (backgrounds in aged care, nursing, public health, occupational therapy, psychology) and healthcare professionals at the site (site manager, clinical care consultant, clinical care manager, nurse leaders, on-call GP, on-call pharmacist) contextualised the pathway to site needs and practicalities. The pathway was then re-assessed for accuracy and adherence to the literature.4
Person-centred care, based on understanding the person’s history and experiences, their likes and dislikes, taking their perspective into account and ensuring collaboration with the person with dementia and their family or nominated decision-maker, underpins the pathway.
‘Risk’ is defined as the potential for harm or danger (physical or psychological) to the person living with dementia or those around them. The degree of risk is assigned
depending on three aspects that need to be assessed together: the severity of the behaviour; the context of the behaviour; and the resources available to manage the situation.
Five risk management stages were identified within the literature as critical to the evidence-based management of changed behaviours in RACFs.3
1. Risk assessment;
2. Prevention;
3. Maintenance;
4. Escalation; and
5. Pharmacological Interventions.
This information was collated into a colourcoded pathway comprising an instruction guide and quick reference flowcharts.4
We conducted a feasibility trial at one memory support unit, during which the pathway became standard practice for five months. Data collection occurred pre- and post-intervention and included surveys, focus groups with staff, and health record audits.
RESULTS
The pathway was successfully adopted and well accepted by nursing and clinical care staff, who indicated the pathway was embedded at the site and will continue beyond the trial period. Overall, staff perceived the pathway had a positive impact on resident wellbeing in relation to decreased behavioural incidents and reduction in antipsychotic use. Staff attributed these in part to a shift in focus from the behaviours themselves to the cause of the behaviour, which changed the culture of dementia management at the site.
Staff also noted increased job satisfaction from using the pathway to find a solution that prevented or deescalated an incident, rather than resorting to medication. Staff reported an increase in communications between site staff, medical professionals, residents and their families and carers, and felt the pathway improved communication about resident care, and improved their confidence in care decisions.
The positive outcomes of the pathway directly influenced staff perceptions of its impact on workload. It was acknowledged that learning the new documentation was
initially a burden. However, by the end of the trial, most felt this was acceptable due to the positive outcomes. Once the new documentation became second nature, the burden dropped, handovers were more structured, and continuity of care improved over time; this was felt to be more effective than previous methods. Staff felt these outcomes reduced workload in other areas as the residents’ dementia symptoms were better managed, so there were less incidents related to changed behaviours.
CO NCLUS ION
The pathway ensured the site was meeting Aged Care Quality Standards audit and reporting requirements with little addition to staff workload. Minor changes were suggested to improve the overall usability and clarity of the pathway and data collection tools. Including care workers and support staff in the pathway implementation was recommended.
NEXT STEPS
A randomised controlled trial is planned to test the pathway more rigorously to see if it can be extended successfully to multiple sites, and if the perceptions of staff at the original test site are repeatable.
This clinical pathway based on current best practice evidence to prevent or manage the onset of dementia related behaviour changes in RACFs was well accepted and adopted by nursing and clinical care staff. The pathway has the potential to improve dementia care, and has demonstrated its potential to be practically applied in a clinical setting.
Funding: Nurses Memorial Foundation of South Australia
Authors
Kate Kennedy, Deborah Forsythe, Greg Sharplin and Professor Marion Eckert are all based in the Rosemary Bryant AO Research Centre, Clinical and Health Sciences, at the University of South Australia. Joanne Wagner is based in the ANMF (South Australian Branch).
References
1. Dementia Australia. Key facts and statistics. Dementia Australia. dementia.org.au/statistics. Updated July 2022. Accessed 2022.
2. Kinsman L, Rotter T, James E, Snow P, Willis J. What is a clinical pathway? Development of a definition to inform the debate. BMC medicine. 2010;8(1):1-3.
3. Kennedy K, Forsythe D, Wagner J, Eckert M. Clinical pathways for the evidence-based management of behavioural and psychological symptoms of dementia in a residential aged care facility: A rapid review. Australas J Ageing. 2021;Dec;40(4):347-355.
4. Kennedy KJ, Eckert M, Forsythe D, Wagner J, Sharplin G. Development of a clinical pathway for behavioural and psychological symptoms of dementia care: A tool to improve resident outcomes. Australasian Journal on Ageing. 2022.
CLINICAL REVIEW Jan–Mar 2023 Volume 27, No. 10 33
Kristen Wischer ANMF Senior Federal Industrial Officer
The Aged Care Work Value decision: What does it mean for you?
On 4 November 2022 the Fair Work Commission (FWC) handed down its decision on the ANMF and HSU’s applications to increase award wages for all employees working in residential aged care and home aged care.

The unions sought an increase of 25% for all classifications. The FWC decided to grant an interim increase of 15% for direct care workers.
The FWC agreed that for direct care workers in the aged care sector, the existing minimum wage rates do not properly compensate employees for the value of the work performed. They found that wages should increase for ‘work value’ reasons. These included:
• The workload of nurses and personal care employees has increased, as has the intensity and complexity of the work.
• The acuity of residents and clients has increased. People are living longer and entering aged care later as they are choosing to stay at home for longer and receive in-home care. Residents and clients enter aged care with increased frailty, co-morbidities and acute care needs.
• There is an increase in the number and complexity of medications prescribed and administered.
• The proportion of residents and clients in aged care with dementia and dementia-associated conditions has increased.
• Home care is increasing as a proportion of aged care services.
• Since 2003, there has been a decrease in the number of RNs and ENs as a proportion of the total aged care workforce. Conversely, there has been an increase in the proportion of PCWs and AINs.
• Registered Nurses have increased duties and expectations, including more administrative responsibility and managerial duties.
• PCWs and AINs operate with less direct supervision. PCWs and AINs perform increasingly complex work with greater expectations.
• There has been an increase in regulatory and administrative oversight of the Aged Care Industry.
• More residents and clients in aged care require palliative care.
• Employers in the aged care industry increasingly require that PCWs and AINs hold Certificate III or IV qualifications.
• The philosophy or model of aged care has shifted to one that is person-centred and based on choice and control, requiring a focus on the individual needs and preferences of each resident or client.
• Aged care employees have greater engagement with family and next of kin of clients and residents.
• There is an increased emphasis on diet and nutrition for aged care residents.
• There is expanded use and implementation of technology in the delivery and administration of care.
• Aged care employees are required to meet the cultural, social and linguistic needs of diverse communities including Aboriginal and Torres Strait Islander people, culturally and linguistically diverse people and members of the LGBTQIA+ community.
The FWC accepted our expert evidence that the skill, responsibility and effort required in the RN, EN and AIN/PCW classifications is under-recognised because it is work performed in a female dominated industry and that gender assumptions have contributed to undervaluation.
So, where to from here?
The FWC recognised there was a need for a wage increase to be passed on as soon as possible, but that it needs more evidence to make a final decision. In the coming months, the parties will try and reach agreement on how the increase will be implemented. The FWC will assist if necessary.
Once the mechanism for passing on the increase has been determined, RNs, ENs, AINs and PCWs on award rates will receive a wage increase of 15% on top of the current award rates. We recognise it is not just award reliant employees who need wages to increase. For employees on enterprise agreements, we are seeking to ensure that the Commonwealth Government agrees to fund increases across the sector, so that everyone gets the benefit of the decision.
We are also advocating for the increase to apply to other classifications, in particular recreation and lifestyle officers, chefs and cooks. There will be the opportunity to bring further evidence for aged care workers not covered by the decision, including gardeners, cleaners and administrative staff.
We are very happy with the outcome of the interim decision, but there is more to be done. How and when the increase will be passed on, the scope of any further increases for nurses and care workers and expanding the outcome for staff in other classifications is important work still to come.
The ANMF will update members on how and when the interim increase of 15% will be implemented in the coming months.
INDUSTRIAL 34 Jan–Mar 2023 Volume 27, No. 10



Earn up to $800* a day as a locum nurse
$800* PER DAY PLUS LOADING AS APPLICABLE *Subject to terms and conditions as outlined
by joining a program that offers the unique opportunity to explore the countryside while helping your peers take a much-needed and well-deserved break. Scan the QR code above to express your interest today.
during the Rural LAP placement process.
Edge of scope practice –what it means for nurses
February 2019 saw the beginning of Victoria’s fourth Gem at Home program, based at Barwon Health. It operates from a dilapidated building, fondly nicknamed the shed, based at the back of the McKellar centre in Geelong.

 By Julie Lavery
By Julie Lavery
Much like the existing programs it is funded as an inpatient ward, and acts as an inpatient unit going to the patient’s home. Consequently, the team is comprised of similar disciplines to a ward. There is a geriatrician and registrar, nurses, physios, occupational therapist, dietitian, pharmacist, ward administrators and podiatrist. Generally the service lasts for about two weeks.
Gem at Home aims to provide medical and restorative care to over 65’s. It works to decentralise healthcare from the usual hospital setting. Obvious advantages of this are seeing the patients’ issues from their perspective from within their home setting, patients are motivated to do the work in order to stay at home and staying away from hospital means staying away from an environment that is potentially disorientating and deconditioning.
The Gem at Home model at most other services, involves multiple visits in a day as each speciality practices its own discipline. This means for example, physiotherapists set and observe exercises, the nurses take blood pressures and attend wound dressing and occupational therapists sight grab rails. A simplification of tasks perhaps but undeniable that this involves potential multiple visits to the patients’ homes each day.
Barwon Gem at Home identified the potential burden of this system. It was perceived that more than one visit per day would impose on the patient’s time and fail to promote independence and resourcefulness.
An edge of scope form of practice for the whole team was therefore developed and put into action, permitting Barwon’s service to provide intensive rehabilitation
and medical care with only one health professional visit per day.
Edge of scope practice celebrates the expertise of each discipline, whilst also acknowledging that there are basic tasks that really any health professional can accomplish. The more routine tasks that were identified initially were observations of blood pressure, pulse, temperature and respirations and performing the physiotherapy prescribed exercises. There are also assessment skills that have grown too, so now a nurse will identify the need for a grab rail or hand held shower in the shower for the occupational therapist to follow up on their visit. A physiotherapist will skin check and if a simple wound is found will cover it with a dry dressing for a nurse to follow up the next day.
During the Gem at Home visit all health professionals, irrespective of discipline will take vital signs, they will complete the prescribed home exercise program with the patient and take them for a walk, ideally outside, function and weather permitting. They will check the patients’ feet and apply the advised cream. Food supply and the ability to prepare and cook will be assessed and of course that they have eaten. The
36 Jan–Mar 2023 Volume 27, No. 10 REFLECTION
Gem at home team
safety of the shower will be assessed early in the admission, and the patient’s hygiene needs and cleanliness will be assessed daily. Each visit, pressure areas will be monitored, with anyone able to highlight risk and respond with an equagel cushion before the resulting occupational therapist visit.
Edge of scope care for nurses develops and expands existing holistic care and assessment skills. There is enormous satisfaction from caring for the whole patient, paying careful attention to their needs and frailties whilst encouraging their improvements. The patient view is opened up to include every system and social need. Nutrition becomes checking for used dishes to suggest the patient has eaten, checking their tongue, taking them shopping if needed and providing meal prep education. It has also elevated the understanding for the allied health team members of
what nurses do. Nurses are more than simple task performers. Their skills and knowledge are celebrated. This might be complex wound care, stoma management, diabetes management, a fluid review, constipation management or a thorough pain assessment.

When Gem at Home patients are admitted, either from the acute hospital or the community they are often quiet unwell and need the clinical oversight of a nurse, or perhaps unfortunately their condition deteriorates during their time on the program. These events dictate a call to the nurse in charge for phone support and triage, deciding whether to immediately escalate to the doctor or 000, visit for review or provide phone advice. It is the nurse whose day must be flexible and responsive, ready to attend unwell patients. The nurse reviews if vital signs are deranged, or
immediately post falls, providing it is not an emergency situation. An occupational therapist in the home of a patient with a blood nose calls and the nurse visits to pack, a dietitian visits and finds a patient’s O2 saturation is 73% dictating a 000 call has a nurse on scene to support patient and clinician and liaise with the medics. Alternatively, a patient with a sudden weight gain of two kilos and shortness of breath may be managed with a prompt nurse review and discussion with the medical team to amend their medications, avoiding a trip into hospital.
What edge of scope means for nurses is a fresh challenge, extending their holistic assessment, earning the respect and acknowledgement of the multidisciplinary team. They are a vital cog in a patient focused service. Edge of scope means a challenging, fun and rewarding job.
Author
Julie Lavery is the Nurse Unit Manager of Gem at Home for Barwon Health in Victoria. Julie has been nursing for 40 years in various acute and subacute settings. Her recent experience is centred around palliative care and particularly community palliative care
REFLECTION Jan–Mar 2023 Volume 27, No. 10 37
What edge of scope means for nurses is a fresh challenge, extending their holistic assessment, earning the respect and acknowledgement of the multidisciplinary team.
Cannula conversations:
An initiative to reduce bloodstream infections
 By Chiane Marshall
By Chiane Marshall
With the aim to reduce the rate of peripheral intravenous catheter (PIVC) related bloodstream infections (BSIs) at the Townsville University Hospital, a six-month quality improvement activity was initiated through education, patient engagement, and surveillance.
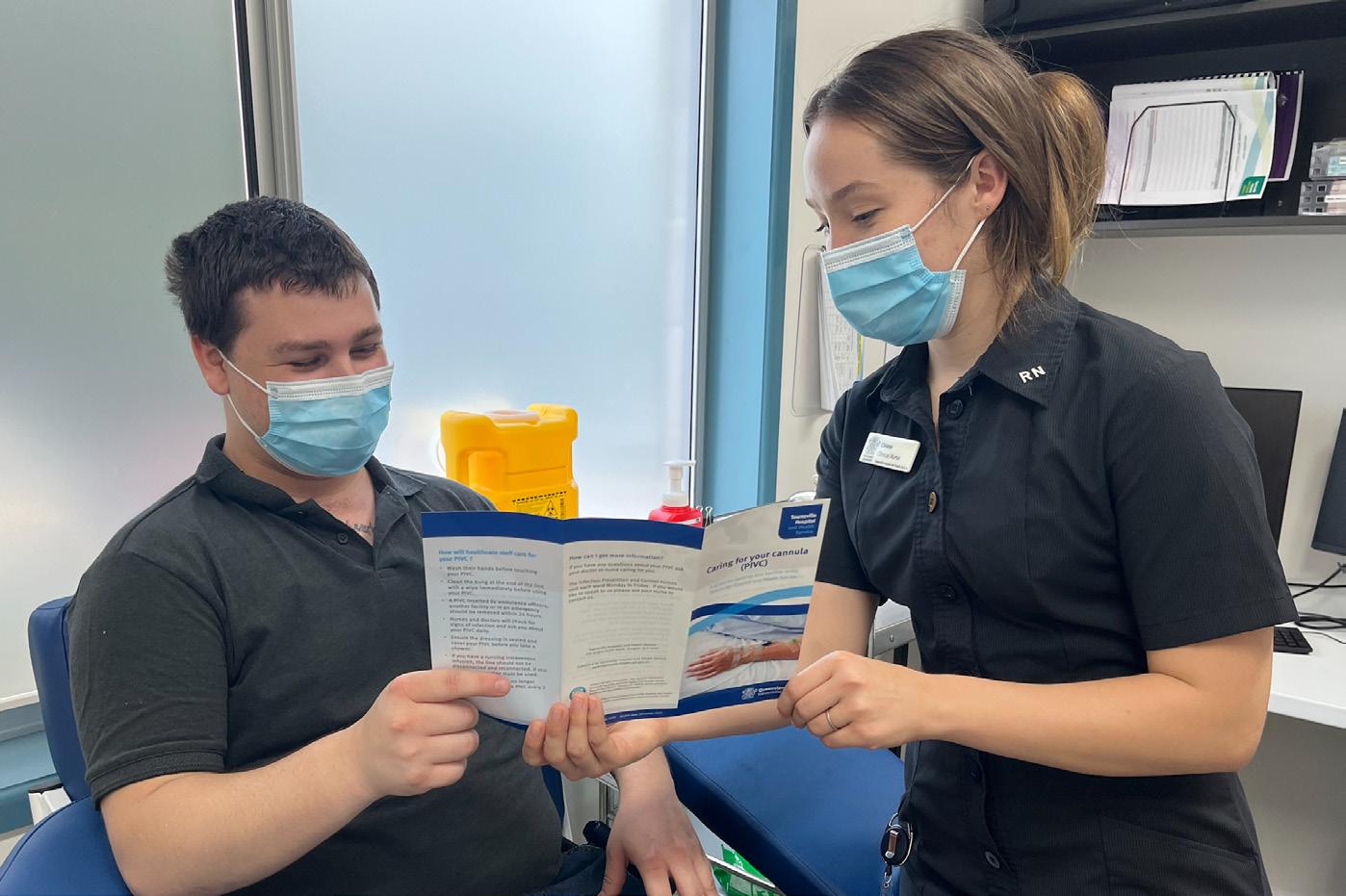
Healthcare-associated BSIs (HA-BSIs) have a significant burden on the healthcare system and are largely associated with increased risk of patient morbidity and mortality.1 Most HA-BSIs are preventable through basic infection prevention and control practices.1 To commit to reducing the issue of HA-BSIs, the Australian Commission on Safety and Quality in Health Care1 released the new ‘Management of PIVCs Clinical Care Standard’ in 2021.
The Townsville Hospital and Health Service (THHS) Infection Prevention and Control Team identified gaps in meeting the new Standard, which included a lack of evidence that inpatients were receiving information about caring for their PIVC, an increase in hospital acquired BSIs in the medical and surgical wards, and poor compliance with routine PIVC documentation.
To reflect the changes from the new Standard the THHS updated the relevant policies, audit tools, and clinical competency assessments. To address the shortcomings, the Infection Prevention and Control Team initiated a six-month quality improvement activity in the medical and surgical wards, which aimed to improve staff education and awareness, patient engagement, rates of PIVC-related HA-BSI, and compliance with documentation.
The interventions included PIVC education for consumers with the support of a ‘Caring for your cannula’ brochure, in-services for nursing staff, and regular audits of PIVC documentation with feedback to the wards.
The results of this activity reflected a positive impact on the rate of PIVC-related HA-BSIs. The rate in the focus wards decreased from 0.67 cases per month
to 0.33 cases per month (eight cases in the 12 months pre-intervention and two cases during the intervention period). In comparison, the wards, which did not receive the intervention had an increase from one case per year to six cases in 2022. Patient education was delivered steadily at an average rate of seven patients per month. Despite delivering 14 ward-based in-services there was no improvement in clinician documentation with the baseline average of 1,361 patients per month with incomplete documentation increasing to 1,374 per month during the intervention period.
These results were impacted by the COVID-19 pandemic, which hindered the team’s ability to enact a consistent implementation strategy. Therefore, education sessions for staff and patients were provided sporadically and ward pressures limited staff ability to attend inservices.
The validity of the HA-BSI data from this activity is limited due to the small sample size, additionally there is no proof of a causal relationship between the intervention and the improvement in HA-BSI rates.
Despite this, the initiative has laid the foundations for further research regarding the barriers to compliance with PIVC documentation and management to inform interventions that may be more effective to implement. Our team is now investigating strategies to effectively implement change and gather more rigorous data.
Author
Chiane Marshall, RN, Clinical Nurse Infection Prevention and Control at the Townsville University Hospital
Reference
1. Australian Commission on Safety and Quality in Health Care. Management of Peripheral Intravenous Catheters Clinical Care Standard [Internet]. Sydney: Australian Commission on Safety and Quality in Health Care; 2021 May [cited 2022 Aug 27]. 54 p. Available from: safetyandquality. gov.au/publications-and-resources/resource-library/ management-peripheral-intravenous-catheters-clinicalcare-standard-2021
“The results of this activity reflected a positive impact on the rate of PIVC-related HA-BSIs. The rate in the focus wards decreased from 0.67 cases per month to 0.33 cases per month.”
ISSUES 38 Jan–Mar 2023 Volume 27, No. 10
Chiane Marshall
Dr Micah D J Peters

Director of the ANMF National Policy Research Unit (Federal Office) and Senior Research Fellow in the Rosemary Bryant AO Research Centre, UniSA Clinical & Health Sciences, University of South Australia
Nursing and midwifery research: With quantity must come quality
Research must be a viable career pathway option for all nurses and midwives. The amount of nursing and midwifery research in Australia is however falling behind that led by other health professions.
Fewer nurses and midwives have opportunities to engage in and lead research particularly when working in busy, clinical roles. This has resulted in a deficit in the quantity of research done by nurses and midwives as evident in the relatively low representation of nursing and midwifery research in Australian competitive grant schemes despite making up more than half of the overall healthcare workforce.
A recent Medical Journal of Australia article focussed on the importance of fostering nursing and midwiferyled research as an investment in healthcare service and patient outcomes.1
It highlighted the need for more nurse and midwife researchers with the training and skills to plan and conduct high quality research. Building research capacity and capability among nurses and midwives must involve enhancing the way research is taught during undergraduate education and follow though to greater availability of opportunities via early and mid-career fellowships and support from employers and funding bodies to enable those working in clinical roles to engage effectively in research.
in research. However, it is likely to be challenging particularly for individuals transitioning into clinical practice following graduation. Undergraduate programs could include additional elective research training for students who are interested in embarking on research and more flexible opportunities to develop research skills in the years following graduation could be implemented.
Elsewhere in this issue, we describe how at the University of South Australia we have been mentoring Vacation Research Scholars from the undergraduate nursing program to undertake small research projects to build knowledge, and confidence in engaging in research.
References
1. Eckert M, Rickard CM, Forsythe D, Baird K, et al. Harnessing the nursing and midwifery workforce to boost Australia’s clinical research impact. MJA. 2022. [Online First]. doi:10.5694/mja2.51758.
2. Halcomb E, Smyth E, Moxham L, Traynor V, et al. Bachelor of Nursing Honours programs in Australia: Current trends and key challenges. Collegian. 2018;25(4):429-434.
3. Schwartz S. Educating the Nurse of the Future Report of the Independent Review of Nursing Education.
Canberra: Commonwealth of Australia. 2019.
Undergraduate nursing and midwifery education should foster the development of research capability and capacity, however research education forms only a small part of degree programs. As the Australian Nursing and Midwifery Accreditation Council (ANMAC) Standards state, undergraduate program content and subject learning outcomes must support the development of research skills including searching and reviewing research and other evidence for translation into practice. These skills, however, do not appear to extend to the more advanced skills of conducting and reporting research. While many universities offer Honours programs which focus on equipping students with additional research skills and experience enrolments are low and declining.2
The Independent Review of nursing education in Australia recommended exploring the potential for moving towards a four year undergraduate degree. However this was not to embed a research-focussed Honours year, but to nest a two year associate degree at the beginning of the program.3
While the ANMF disagrees with the creation of a four year undergraduate degree, it has no position for or against an optional Honours degree for graduates. This Honours year might be an optimal forum for new graduates who want to build skills and experience
Alumni have focused on diverse topics from best practice care for gender and sexually diverse people in emergency departments to the work values of generation Z nurses. Such programs leverage existing funding schemes to enable students to undertake work with us over the vacation period and are likely to help create pathways to postgraduate study and early career research. By utilising similar opportunities, academics can help foster research skills by building on what is taught in undergraduate courses and creating both a pipeline to further study as well as valuable collegial relationships with emerging research leaders.
Opportunities for joint appointments between academic and clinical sectors would also enhance both the number of nursing and midwifery academics and the number of research-engaged staff working in health, further embedding research expertise in clinical practice, and strengthening links between evidence generation and synthesis, implementation, and evaluation.
It is hoped that with various advancements to further support Australian nursing and midwifery research, including initiatives such as the Australasian Nursing and Midwifery Clinical Trials Network and Stream 1 of the Medical Research Future Fund, that nursing and midwifery research will take on new prominence. With quantity must come quality too, and over the coming years, I and my colleagues will be looking to build and sustain further opportunities for nurses and midwives to gain confidence and skills engaging in and leading high-quality research through exploring how to support both undergraduate and post graduate students and experienced clinicians alike.
RESEARCH & POLICY Jan–Mar 2023 Volume 27, No. 10 39
What does building capacity look like in the school nurse setting?
An opinion on high school/college nursing
By Leah Furley and Lisa Evans
The role of the school nurse in Tasmania is diverse, the primary role being health promotion and health education.

School Health Nurses provide health advice, referrals, education, and support to students, families, and wider community. Anecdotally, moving from a health setting to an education setting many school nurses feel it is difficult to measure the impact of their interventions.
Coming from a health setting where the evidence of your intervention is immediately evident and interventions are predominantly ‘doing’ in nature ie. administering analgesia,
applying a plaster of paris, the move to working in a primary health role is quite a shift. This fact combined with an innate desire to help can at times leave us wanting to step in, taking ownership and responsibility for a student’s health.
There is however a different approach, rather than ‘doing’, we can be encouraging our students to take ownership of their own health by building their capacity. In such a diverse and challenging environment how well have we changed our ways of working so far?
The term capacity building1 is the ability to tap into the existing capabilities of
individuals, communities, organisations, or systems to increase involvement, decision making and ownership of issues.
As school health nurses we are perfectly placed to adopt a capacity building approach and promote health ownership amongst our students. Vic Health suggests that working in capacity-building ways benefits the confidence, knowledge, skills, and self-efficacy of patients (students).
Encouraging capacity building in clients was identified in nurse Orem’s Self-Care Deficit Theory.4 Orem4 defines nursing as helping others while encouraging self-care.
VIEWPOINT 40 Jan–Mar 2023 Volume 27, No. 10
School Health Nurse Leah Furley.
Orem4 is not alone in her observation on the benefits of encouraging capacity building2 suggested that a key component of building capacity is collaboration, building trust and assisting to increase independence3 refers to the nurse as a coach suggesting that the best person to manage one’s own health is the patient and that nurses are often in the best position to promote this. This concept can easily be applied in the school nurse setting.
The skills required to be an effective coach; questioning, effective listening and giving feedback, are skills that can be developed and used daily by school health nurses. An example of this is working with individual students to plan goals that will promote responsibility such as teaching students about good sleep hygiene and then guiding them to implement a SMART goal around this or teaching students how to access free health and community services such as Family Planning or Headspace.
Implementing capacity building is not without its challenges, lack of time, education and understanding can all impact on how well capacity-building is implemented in the school setting.
Helicopter parenting is a term used to describe parenting where the parent makes all the decisions, children are not given space to develop their own problem-solving or decision-making skills, and where children are not taught to be independent.3P73 The consequences of this well-intentioned parenting style include neuroticism, being less open to new experiences, increased dependence, and decreased psychological wellbeing.3P73
Like helicopter parenting, ‘helicopter nursing’ arises from a desire to help, but also doesn’t support students to make their own decisions, doesn’t encourage problem-solving, and does not teach independence. We suggest that the consequences of this style of nursing will likely increase students’ dependence rather than building their own individual capacity to care for their own health and wellbeing. School
health nurses are often faced with students requesting support to access external services. Well-intentioned school nurses, new to the program may make the phone call, and arrange the transport and a chaperone. However, by adopting a capacity-building approach they could spend time coaching students to increase their capacity and independence, ultimately benefiting the student in the long term.
We propose that building capacity in our students is the way forward. Working in capacity-building ways is recognised by the school health nurse program as an integral component of working with young people and their families.
Our school nurses now support each other to increasingly work in capacity-building ways, senior nurses share their experiences in weekly nurse ‘huddles’ and through peer support.
The School health nurse program has not existed in its current form for very long but we are excited to be a part of the program and intend to continue learning new ways of working for the benefit of our students.
Authors
Leah Furley RN and Lisa Evans RN are both School Health Nurses for the Department for Education, Children and Young People in North west Tasmania.


As school health nurses we are perfectly placed to adopt a capacity building approach and promote health ownership amongst our students.
References
1. Victorian Health Promotion Foundation 2012, Capacity building fact sheet, publication number: C-072-CB, viewed 01 November 2022 vichealth.vic.gov.au/-/ media/ResourceCentre/ PublicationsandResources/ General/Capacity_Building_ FactSheet.pdf?la=en&hash= 28D731AE5A13A61534 865272CF8A3534DAA9954D
2. Hughes S. Promoting independence: the nurse as coach. Nursing Standard. 2003 Nov 19-25;18(10):42-4. PMID: 14679659.
3. Benedetto L. 2021, Parenting –Studies by an ecocultural and transactional perspective, IntechOpen, London, UK
4. Petiprin, A, 2020, Orem’s self-care deficit theory Accessed: 01 November 2022. nursing-theory.org/theoriesand-models/orem-self-caredeficit-theory.php
VIEWPOINT Jan–Mar 2023 Volume 27, No. 10 41
School Health Nurse Lisa Evans Leah Furley and Lisa Evans


More Information: Credit criteria, fees and charges apply. Offer is current as of 10 October 2022. 1. Lower amounts and LVR apply depending on property type and location. Funds to cover transaction and establishment costs are required. Genuine Savings are not required to be evidenced under the Medico guidelines to a Max LVR of 90%, where the application does not qualify for Medico loan and LVR > 85%, evidence of 5% genuine savings is also required. Owner Occupied interest only loans have a maximum LVR of 80%. Investment loans have a maximum LVR of 90%. 2. The qualifying professionals’ gross taxable income must be a minimum of $90,000pa. Eligible income must be earned from the applicants’ profession or qualification (i.e. cannot include proposed or existing rental, interest, dividends etc.). Qualification must be confirmed in all instances via a copy of either the University degree or qualification, or Registration with the Medical Practitioners Board of Australia or equivalent body. RAMS Financial Group Pty Ltd ABN 30 105 207 538, AR 405465 Australian Credit Licence 388065. Credit Provider & issuer of RAMS Deposit Products: Westpac Banking Corporation ABN 33 007 457 141 AFSL and Australian credit licence 233714. 23097/1122 HIRING URSES MAKE YOUR NEXT CAREER MOVE Why Choose Altaira? Job security Opportunities for further career advancements Free training 24/7 clinical support and family friendly culture Access to mental health and wellness initiatives

UNDERGRADUATE NURSING & MIDWIFERY STUDENTS AND GRADUATE TRANSITION TO PRACTICE Jan–Mar 2023 Volume 27, No. 10 43 FOCUS
Innovative practices within a Transition to Professional Practice Program to support workforce challenges
By Caterina Feltrin
In 2019 stakeholder engagement was undertaken to redesign the Transition to Professional Practice Program (TPPP) curriculum across a Local Health Network (LHN).
The new curriculum was developed to meet the education and support needs of the novice registered nurses (RNs) and was successfully implemented in 2020. When program planning for 2022 commenced, the aim was to stay aligned with the new curriculum and program structure however, several workforce challenges had presented that impacted the program delivery:
• An increase in commencing TPPP participants from 190 to 250 to address staffing/workforce/rostering deficits across the LHN.
• An exponential increase in participants requesting a reduction in their contracted hours to preserve wellbeing whilst navigating being a novice nurse during the Covid-19 pandemic.
• An increased need for clinical and bedside support from Clinical Nurse Educators (CNEs) at the commencement of employment.

To accommodate these workforce challenges, some practical and innovative adaptations were made to the TPPP structure whilst still meeting curriculum requirements.
As a result of increased participant numbers located across eight sites within the LHN, additional CNEs were recruited to maintain the same level of clinical support provided in previous years. A creative approach was required to ensure equitable support to the participants, dividing the CNEs into teams and evenly allocating participants among them. This new strategy generated multiple benefits, such as oversight of a smaller number of participants proved more manageable and communication within each CNE team was more efficient. In addition, the CNE team approach has allowed for increased capacity to build rapport with each participant and subsequently provide individualised support.
Changes to the organisation’s orientation were implemented to include a twoday hospital orientation, one unit/ward orientation day and four supernumerary days. Previously, participants would receive as little as one supernumerary shift before expecting to take a patient load independently. The unit/ward orientation day allows Program Nurse Educators (PNEs) to induct participants to their allocated
ward affording the time and space for familiarisation with the ward environment. In addition, program/speciality specific education was provided. Feedback from PNEs and Nurse Unit Managers indicated that the increase in supernumerary days has increased participant readiness to safely manage a patient load on their first independent shift.
All participants onboarded for 2022 were offered a part-time contract only (four days per week), resulting in several opportunities and positive outcomes. Part-time hours provided the opportunity to implement the program structure differently, reducing five full Professional Development Days (PDDs) to three PDDs and three workshops. On a rostered day off, participants attended the 3.5-hour workshops and were paid for their time post-attendance. This novel solution allowed time for participants to attend education whilst not impacting their ward rosters. This also allowed participants to choose when to attend workshops via an online booking system, increasing flexibility and allowing for differing transition rates. It is anticipated that the shorter education sessions will also increase participant learning and engagement. Additionally, decreasing the number of PDDs that are rostered study days increases the number of days worked on the ward. These operational changes to TPPP education delivery proved to be significant in preserving staffing numbers and reducing roster pressure resulting from the large number of nurses required to furlough due to Covid-19 guidelines.
Resulting from reduced contract hours, participants have reported experiencing a manageable work-life balance, and there has been a decrease in the number of requests to reduce contracted/work hours. Two more TPPP intakes are expected for 2022, and extensive evaluation is planned to capture the outcomes of changes implemented. There are early indicators that the changes are leading to positive outcomes for TPPPs, CNEs, Nurse Educators and Nurse Unit Managers.
Author Caterina Feltrin Master of Nursing (Education), Graduate Diploma in Nursing, Bachelor of Nursing, Bachelor of Health Sciences is a Nurse Educator, Early Career Transition Programs, Central Adelaide Local Health Network and Nurse Educator, TPPP Project, Australian Nursing and Midwifery Federation (SA Branch)
FOCUS 44 Jan–Mar 2023 Volume 27, No. 10
Supporting novice nurses in an Early Career Transition Program
By Jenna Georgacopoulos
The Supported Registered Nurse Program (SRNP) and Supported Enrolled Nurse Program (SENP) are six-month Early Career Transition Programs (ECTP) for registered and enrolled nurses who have not previously participated in or have not been accepted into a transition program.

The program is closely aligned with the existing Transition to Professional Practice Program (TPPP) and aims to provide new nurses access to additional clinical support and education. With an ever-increasing junior nursing workforce, the need to support novice nurses is imperative, especially those new to acute care. Support is not only for ensuring consumer safety but for successful transition and staff retention within the health network.¹
The ECTP focuses on newly graduated, novice and new to acute care nurses with the aim to support the successful transition from novice to advanced beginner in nursing practice. The ECTP consists of the TPPP, Supported Registered Nurse Program and Supported Enrolled Nurse Program. With limited positions within the TPPP, paired with increased onboarding of nurses with little or no experience, the need to fill the gap to ensure all staff receive adequate support is evident.
A dedicated referral form for the program with screening questions was designed and implemented in 2022 to facilitate Nurse Managers and Nurse Educators within the
network to identify and refer new staff to the programs easily.
This referral form also asks for agreement to support the participant to attend the required professional development sessions to ensure successful completion of the program.
The link is emailed to the appropriate audience and made available on the Learning Management System for easy access. Before this, there was no formality in the referral process, which was often completed via email.
The SRNP and SENP provide a range of education and clinical support activities.
Clinical visits by Clinical Nurse Educators (CNEs) allow for practical bedside teaching, professional role modelling and wellbeing check-ins.
Professional Development Days provide an opportunity for more formal learning, connecting with colleagues, reflection and debrief in a safe, non-clinical environment.
Short workshops are also offered for targeted, more intense learning whereby pre-learning is completed before attendance and applied through the 3.5-hour workshops
onsite. These workshops strongly emphasise detecting and managing the deteriorating patient and increasing participants’ confidence in systematically assessing patients. Cultural safety and wellbeing are also a key focus.
In previous years the SRNP and SENP saw approximately 25 to 30 acute care nurses transition per six-month program. Currently, the programs have 140 participants, as well as an extensive waiting list. This significant increase reflects increased awareness of the program, its reputation, a streamlined referral process, and an influx of new nurses being onboarded to fill the staffing deficit experienced within the acute healthcare setting.
It is hoped that support and resourcing for these programs continue to grow as their benefits to consumers, staff, and the organisation become more evident. By investing time and resources into the transition of novice nurses now, the organisation is investing in the future through retention of a knowledgeable and experienced nursing workforce.
Author
Jenna Georgacopoulos Graduate Certificate of Nursing (Education), Bachelor of Nursing is Nurse Educator, Early Career Transition Programs, Central Adelaide Local Health Network, Royal Adelaide Hospital, South Australia
Reference
1. Russell K, Juliff D. Graduate nurse transition programs pivotal point of participants’ practice readiness questioned during the COVID-19 pandemic crisis: A scoping review. The Journal of Continuing Education in Nursing [Internet] 2021 Aug [cited 2022 Jul 18]; 52(8), 392–396. Available from doi. org/10.3928/00220124-20210714-09
FOCUS Jan–Mar 2023 Volume 27, No. 10 45
A new resource to teach culturally-responsive palliative care for Australian Indigenous peoples
By Kylie Ash and Sharon Wetzig
The Palliative Care Curriculum for Undergraduates (PCC4U) project team recently launched the Focus Topic Toolkit: Caring for Australian Indigenous peoples affected by life-limiting illness
Purpose-built for Australian entry-topractice health professional students, the resource supports developing the knowledge and skills to provide quality care for Australian Indigenous peoples with life-limiting illnesses and their families and communities.
The Toolkit supports holistic and culturallyresponsive care. Nursing students will recognise the important role they play in breaking down the access barriers to mainstream healthcare experienced by Australian Indigenous peoples. They are provided with opportunities to reflect on a living and flexible service delivery model and consider how their practice can support this.
The Toolkit aims to promote understanding and reframing of palliative care in Indigenous ways of knowing, being and doing. It has been developed collaboratively with Australian Indigenous and nonIndigenous educators, researchers, and clinicians. Learning includes strengths based approaches, use of narratives, reflective activities that support the
development of humility and respectful healthcare practice and an understanding of rights-based pedagogy. Nicole Hewlett, a Palawa woman from Lutruwita (Tasmania) and National Indigenous Manager for the IPEPA program, supported the development of this resource, stating, “Resources are often written about us, without us – which means our voice is lacking along with true knowledge and education. This toolkit has been decolonised and built again from the ground up, on foundations of the sovereign spirit of our people.”
The learning outcomes for this resource align with key Australian strategies and frameworks:
• The National Scheme’s Aboriginal and Torres Strait Islander Health and Cultural Safety Strategy 2020- 2025, Australian Health Practitioner Regulation Agency.
• The Nursing and Midwifery Aboriginal and Torres Strait Islander Health Curriculum Framework: an adaptation of and complementary document to the 2014 Aboriginal and Torres Strait Islander Health Curriculum Framework, Congress of Aboriginal and Torres Strait Islander Nurses and Midwives.
• IAHA Cultural-responsiveness Framework, Indigenous Allied Health Australia.
• Aboriginal and Torres Strait Islander Health Curriculum Framework, Department of Health.
• Graduate Capabilities in Palliative Care, PCC4U.
Educators who reviewed the resource in development commented:
“The resources are contemporary, relevant, and provocative for many students, which is good – it can elicit deep learning.”
– Academic, Nursing
“The tone of the entire toolkit is really affirming and encourages people to participate. “
– Academic and Clinician, Medicine Health students who reviewed the Toolkit in its finalised form commented:
“The content made me reflect quite a bit on my own biases and trying to come up with ways as health professionals that we can improve Indigenous palliative care issues.”
– 4TH year Student, Paramedicine and Nursing
“As an Aboriginal person, I found the information to be extremely respectful, thorough and safe… It’s the truth and it does not fabricate the experiences of Indigenous people.”
– 4TH year Student, Social work
The Toolkit and all learning resources are available to educators and students at no cost and accessible at pcc4u.org.au
For any further information on the toolkit implementation, please contact the project team at pcc4u@qut.edu.au
Authors
Kylie Ash, PCC4U Project Manager, Cancer and Palliative Care Outcomes Centre, QUT
Sharon Wetzig, PCC4U/PEPA Learning and Development Coordinator, Cancer and Palliative Care Outcomes Centre, QUT
PCC4U Focus Topic 2 Title Page PCC4U Focus Topic 2 Toolkit Content FOCUS 46 Jan–Mar 2023 Volume 27, No. 10
Preparation of student nurses for registration and healthcare delivery
By Felicity Walker, Nicola Whiteing and Christina Aggar
Nursing workforce shortages and continuing pressures on healthcare systems require health services and education providers to work collaboratively to support student nurses’ transition into practice, preparing and retaining a quality nursing workforce.
In recognition of this, a regional tertiary education provider has partnered with a NSW Local Health District (LHD) to conduct a longitudinal mixed method study evaluating a cohort of Bachelor of Nursing (BN) students completing placement at a NSW LHD. The study is to determine the preparation of student nurses and their retention within the nursing workforce. As part of this larger study, the collaborative partnership
implemented a Work Integrated Learning Community (WILCo) model in which a cohort of BN (n=28) students experienced all of their clinical placements (8) within a single facility. A longitudinal qualitative approach was used to evaluate the student’s experience within the WILCo model. Clinical placement is imperative to supporting the development of student nurses’ critical thinking and decisionmaking skills and their ability to apply their skills and knowledge in practice.1 Poor or negative experiences can impact the student’s intention to remain in the program and also their transition into clinical practice.2,3 Student attrition impacts inflow into the nursing workforce, and poor retention of new graduates is an economic burden and drains nursing workforce capacity.4 Due to this, there is a need for studies to ascertain the reasons behind a nurse’s decision to remain in or leave their undergraduate training, clinical area, or the nursing profession.
This collaborative study focuses on different aspects of the clinical placement experience and transition into practice. The WILCo arm of the study explored a new model for clinical placements in the local area. Results found that consistency in placement settings provided:
• quality learning experiences;
• created a sense of loyalty;
• reinforced the intention to remain with the organisation;
• built student confidence;
• enriched student’s linking of theory to practice;
• reduced student anxiety;
• fostered a sense of belonging and team membership in the healthcare setting; and
• developed a support network and collegiality among student peers.
As a result of this, the WILCo program is continuing and is being rolled out with other healthcare services connected to the education provider. This study is significant in contributing toward the retention of nurses and ensuring a workforce fit for practice.
Authors
Dr Felicity Walker PhD, BNursing (Hons), GradCertCritCareNurse is a Lecturer at Southern Cross University, Faculty of Health, Gold Coast Airport, Qld

Dr Nicola Whiteing PhD, RN, SFHEA, Southern Cross University, Faculty of Health, Gold Coast Airport, Qld Associate Professor Christina Aggar RN BN(HONS), GRAD CERT HE, PhD is Professor, Nursing Research Conjoint Northern NSW Local Health District, Nursing and Midwifery Directorate Southern Cross University, Faculty of Health, Gold Coast Airport, Qld
References
1. Algoso M, Ramjan L, East L, Peters K. Undergraduate nursing assistant employment in aged care has benefits for new graduates. Journal of Advanced Nursing. 2018;74(8):1932-54. doi. org/10.1111/jan.13691
2. Chan ZCY, Cheng WY, Fong MK, Fung YS, Ki YM, Li YL, et al. Curriculum design and attrition among undergraduate nursing students: A systematic review. Nurse Education Today 2019;74:41-53. doi.org/10.1016/j.nedt.2018.11.024
3. ten Hoeve Y, Castelein S, Jansen G, Roodbol P. Dreams and disappointments regarding nursing: Student nurses’ reasons for attrition and retention. A qualitative study design. Nurse Education Today. 2017;54:28-36. doi.org/10.1016/j. nedt.2017.04.013
4. Health Workforce Australia. Australia’s future health workforce – nurses overview. 2014.
FOCUS Jan–Mar 2023 Volume 27, No. 10 47
Ashleigh Woods, RN/Midwife. Preparing and retaining the nursing workforce – keeping nurses and midwives in the profession. Photo credit: Southern Cross University
Nursing student and RUSON gains on-thejob experience
By Robert Fedele
When second-year nursing student Scott Li isn’t studying, he’s likely working shifts at Mildura Base Hospital, helping to ease the load and gaining invaluable on-the-job experience before he graduates.

The La Trobe University student is one of many Registered Undergraduate Students of Nursing (RUSONs) working across the state’s public hospitals and health services. Under the paid workforce model, students work under the direct supervision of registered nurses to help provide patient care, typically carrying out tasks such as patient showering and dressing, feeding, manual handling and mobility.
Scott, originally from China, moved to Australia in 2021 and chose to pursue nursing because he wanted to contribute to healthcare amid the COVID-19 pandemic and knew the profession was facing looming shortages that meant jobs would be available.
The 32-year-old mature-age student jumped at the chance to become a RUSON in the hope of fast-tracking his nursing journey. Since January, he has clocked on for three to five shifts per week on the hospital’s surgical ward.

“Mainly, I just assist every nurse, but usually it’s the ones that have very confused or challenging patients such as those who have
dementia or have undergone a big surgery and cannot move at all,” Scott says.
“I help the nurses to roll them over in bed, give them a wash in bed, and help them to go to the toilet. When it’s busy, I’ll take patients’ blood pressure and basic vital signs and even help them with feeding, eating breakfast and lunch, pretty much the basic stuff.”
Scott believes the RUSON program has helped him develop skills, improve time management, and become more prepared to become a registered nurse.
“I think the program really gives you handson experience,” says Scott.
“It’s showed me that hospital environment because eventually, that’s where most of us will end up working, and also you get so much exposure to what you’re going to do in the future.
“As a RUSON, we can take blood sugar and blood pressure, things we just don’t do so much of in school, so if we can get some experience in the job, I think that is really beneficial to us after our graduation.”
Being thrust into the profession amid the COVID-19 pandemic has not been without its challenges, yet, Scott suggests he has managed to cope well with the added complexities.
“There’s just more pressure,” he says.
“It’s also very uncomfortable because you’re wearing a thick mask for eight hours or longer and running around with confused dementia patients that can’t see your face and can’t see your facial expressions and can’t hear you if they have hearing loss. During COVID, we had to put on a gown before we walked into the room. Putting them on and
taking them off is very time-consuming and extremely uncomfortable, but I think it has also offered me an insight into how to manage all this if the next one [wave] comes along, so I’m sure I’ll be better prepared.”
Earlier this year, as part of its 2022/23 Budget, the Andrews Labor Government committed a further $59 million to 2,250 RUSON positions over two years, and $9.8 million to support 75 registered undergraduate student midwives (RUSOMs) per year.
Since the program was launched in 2016, the RUSON/M student employment model has seen more than 3,000 students work across the state’s hospitals.
Scott, who plans to apply for a graduate position at the Mildura Base Hospital once he completes his studies, says the program has made him more confident as he works towards entering the profession.
His advice to nursing students considering applying to become a RUSON is to do their homework and give it a go.
“You need to be prepared because once you’re here [the hospital], yes, you’re a student, but most of the time, you’re also an employee,” he says.
“You will encounter a lot of challenges, but just be open-minded about it. Don’t be frustrated. Because sometimes it can be hard and it can be very challenging. You have patients yelling at you, confused patients even becoming aggressive towards you. So just keep in mind that is only part of the job, and if you’re determined to become a nurse, this is what’s going to happen to you at some point in the future. Be open-minded about this and see it as an opportunity to gain experience.”
FOCUS 48 Jan–Mar 2023 Volume 27, No. 10
Left and right: RUSON Scott Li
Transition to practice: Capability
By Carey Mather and Kathleen Tori
graduate nurses
An integrative review of graduate nurses’ capability upon entering the workforce revealed that workplace readiness expectations have not changed. Research also found there continues to be a lack of consensus on the expected attributes of newly graduated registered nurses.1



The study used a pragmatic approach to develop the research question, define capability, and work readiness and undertake the review.2 Four main themes emerged, knowing and doing, professional behaviour, personal attributes, and organisational acumen. The findings demonstrate the continuance of tension between new graduate expectations and the reality of work.
The COVID-19 pandemic has accelerated the need for further research regarding capability at graduation so clinicians and graduate nurses understand the reality of transitioning to practice. Safe, high-quality, and effective nursing programs of study urgently need to support newly graduated nurses and ensure workforce retention while assisting with preventing moral distress and burn-out of nurses already in practice.3 Educators are vested with preparing students by scaffolded theoretical underpinnings and skill acquisition for nursing subjects and the development of employability skills. Clinicians expect newly graduated nurses to seamlessly fit into teams and demonstrate a broad range of knowledge, skills,
attributes, and behaviours – which often remain unarticulated until graduate nurses do not meet expectations or identify they are overwhelmed.4 More than 20 years ago, Duffield and Lumby5 identified student nurses need to be educationally prepared for best practice while understanding the realities of practice. How do we reach a consensus on graduate nurses’ capability as a profession? Once entry-level expectations are acknowledged, they can be used to support and enable newly graduated nurses’ opportunities to flourish while transitioning and learning in practice and minimising the exodus that is occurring.
References
1. Saghafi F, Bromley P, Guzys D et al. Graduate nurses’ capability upon entering the workforce: An integrative review, Nurse Education Today Volume 121 (2023) 105659. doi. org/10.1016/j.nedt.2022.105659

2. Whittemore R, and Knafl K. 2005. The integrative review: Update methodology. Journal of Advanced Nursing, 52, 546-553. doi:10.1111/j.13652648.2005.03621.x
3. Guzys D, Tori K, and Mather C. 2021 Community health nursing as an exemplar of moral distress. Australian Journal of Primary Health doi. org/10.1071/PY20276
4. El Haddad M, Moxham L, and Broadbent M. 2017. Graduate nurse practice readiness: A conceptual understanding of an age-old debate. Collegian, 24(4), 391-396.
5. Duffield C, and Lumby J. 1994. Caring nurses: the dilemma of balancing costs and quality, Australian Health Review, 17(2), 72-83.
of
–Are we promoting realistic expectations?
Authors
Dr Carey Mather RN BSc GCert ULT GCert Creative Media Technology GCert Research PGrad Dip Health Promotion MPH PhD MACN FAIDH FHEA is Senior Lecturer at the Australian Institute of Health Service Management, College of Business and Economics, University of Tasmania, Launceston Tasmania Professor Kathleen Tori PhD NP MACN FACNP, is Head of Nursing, Health and Education at Torrens University Australia, Melbourne, Victoria
Photo credit: Torrens University Image Library, 2022
FOCUS Jan–Mar 2023 Volume 27, No. 10 49
Innovation in simulation during COVID-19 in the School of Nursing, QUT
 By Sandra Johnston, Lori Delaney, Pauline Gillan, Naomi Tutticci, Karen Theobald and Joanne Ramsbotham
By Sandra Johnston, Lori Delaney, Pauline Gillan, Naomi Tutticci, Karen Theobald and Joanne Ramsbotham
COVID-19 has created widespread disruption to nursing education. Our program, like many others, has been affected by clinical placement cancellations and interruptions to student learning. Despite these hardships, opportunities have been generated for innovation in education. In this instance, we adapted our traditional approach to simulation within the Bachelor of Nursing course, which benefited all involved.
Simulation is well embedded within our course as a learning activity that students complete prior to progressing to clinical placement. Simulation classes typically involve four students participating in a clinically based scenario, responding to patient cues, assessing and deciding on a clinical course of action, with four students observing the engaging simulation. All students participate in a postsimulation debrief led by the simulation facilitator. Ideally, a subsequent clinical placement would provide the opportunity to practice and consolidate skills learned during simulation. Research has demonstrated that an inability to refresh and practice a learned skill repeatedly leads to skill decay in as little as four to six weeks.1 During COVID-19, the
frequent pausing, restarting and even cancelling clinical placements impacted students’ opportunity to practice the transfer of clinical skills learnt/ established during simulation classes. With the uncertainty of further clinical disruptions, nursing academics reconceptualised delivery of simulation to maximise learning. We did this using a method of mastery learning, which required a re-imagination of traditional simulation approach. Mastery learning is a robust, evidence-based teaching methodology designed to improve the acquisition of procedural skills, with the aim of supporting all learners to achieve an agreed standard.2 Mastery learning includes repetitive performance and rigorous assessment of motor skills with specific instructional feedback focused on improving skill performance.3 The learner does not progress to a new skill until the previous one is mastered.4 This form of repetitive practice, implemented and moderated by an expert facilitator, develops clinical reasoning and skills and is associated with greater skill retention.5,6 In the mastery simulation, students were required to demonstrate the skills involved in a comprehensive ‘A to E’ patient assessment. Each time a particular assessment component was not performed or performed incorrectly, the simulation facilitator paused the simulation, conducted a micro-debriefing, and provided immediate feedback. The simulation resumed, and the real-time feedback allowed students to implement changes there and then. Each student was able to correctly complete a comprehensive A to E assessment of a simulated deteriorating patient.
We trialled this mastery simulation approach within a cohort of second-year students. Evaluation of this mastery method found a greater level of student engagement and ease of interaction than our traditional approach. The relationship with the simulation facilitator was perceived to help correct and reinforce correct skill techniques rather than a judgement-based approach. From the facilitator’s perspective, when feedback was provided in real-time to students, there was an improvement in student performance and confidence. This observation has provided preliminary evidence that this simulation method suits students. The simulation research group is currently undertaking a larger study using this method and evaluating skill retention and competency in the School of Nursing.
Authors
Sandra Johnston RN, PhD is Director of Clinical Partnerships in the School of Nursing at Queensland University of Technology
Lori Delaney RN, MN, is Lecturer in the School of Nursing at Queensland University of Technology
Pauline Gillan is Senior Lecturer in the School of Nursing, Paramedicine and Health Sciences at Charles Sturt University
Naomi Tutticci is Senior Lecturer in the School of Nursing & Midwifery at Griffith University
Karen Theobald RN, PhD is Academic Lead-Education in the School of Nursing at Queensland University of Technology
Joanne Ramsbotham RN, PhD is Undergraduate Course Coordinator in the School of Nursing at Queensland University of Technology
References
1. Johnson CE, Kimble LP, Gunby SS, Davis AH. Using deliberate practice and simulation for psychomotor skill competency acquisition and retention: a mixed-methods study. Nurse Educator. 2020 May 1;45(3):150-4.
2. Scahill EL, Oliver NG, Tallentire VR, Edgar S, Tiernan JF. An enhanced approach to simulationbased mastery learning: optimising the educational impact of a novel, National Postgraduate Medical Boot Camp. Advances in Simulation. 2021 Dec;6(1):1-0.
3. Ericsson KA. Deliberate practice and the acquisition and maintenance of expert performance in medicine and related domains. Academic Medicine. 2004 Oct 1;79(10):S70-81.
4. Gonzalez, L., & KardongEdgren, S. (2017). Deliberate practice for mastery learning in nursing. Clinical Simulation in Nursing, 13(1), 10-14.
5. Gillan PC, Delaney LJ, Tutticci N, Johnston S. Factors influencing nursing students’ ability to recognise and respond to simulated patient deterioration: a scoping review. Nurse Education in Practice. 2022 Apr 20:103350.
6. Palmer TJ, Chisholm LJ, Rolf CG, Morris CR. Deliberate practice and selfrecorded demonstration of skill proficiency: One baccalaureate nursing school’s response to the COVID-19 pandemic. Nurse Education in Practice. 2021 May 1;53:103071.
The deteriorating patient manikin
FOCUS 50 Jan–Mar 2023 Volume 27, No. 10







3 Buffalo Court Berwick VIC info@safe-super.com.au INVEST IN YOUR FUTURE I N V E S T S A F E L Y REACH OUT TO LEARN MORE With property prices now rising, don't wait too long U S E Y O U R S U P E R O R H O M E E Q U I T Y 1 0 Y E A R R E N T A L I N C O M E G U A R A N T E E P A Y L O W O R N O T A X O N I N C O M E O N G O I N G P R O P E R T Y M A N A G E M E N T Purchase an investment Purchase an investment property in Melbourne's property in rapidly expanding rapidly expanding South East for South $1,000 deposit. $1,000 deposit. Select 4-bedroom property investments are more stable and profitable than investments in shares. ( 0 3 ) 9 7 0 2 2 5 9 5 SAFE-SUPER COM AU APPLY NOW FOR 2023 Master of Nursing (Clinical and Non-Clinical specialisations) Master of Mental Health Nursing* Master of Nursing (Nurse Practitioner)* Master of Midwifery Practice* Graduate Diploma in Child, Family and Community Nursing Continuing professional development program *online course La Trobe Nursing GO FURTHER IN YOUR NURSING CAREER La Trobe University CRICOS Provider Code Number 00115M
By Seung A (Sarah) Park, Rebecca Sharp, Marion Eckert, Belinda Clark and Micah DJ Peters
Supporting undergraduate nurses and new graduates to transition to the workforce is vital. The global nursing shortage was widely apparent even before the COVID-19 pandemic. The WHO estimated a shortfall of 5.9 million, necessitating 10.6 million nurses by 2030, as almost 17% of nurses are expected to retire over the next decade.1
Alarmingly, the International Council of Nurses predicts an even greater global nursing deficit of about 13 million following the COVID-19 pandemic due to nurses leaving the profession.2
Nursing workforce shortages are also exacerbated when new graduates leave the workforce or don’t find jobs. New graduates can experience feelings of unpreparedness and stress during their transition to professional practice.3,4 These issues can reduce new graduates’ job satisfaction and confidence, resulting in a high turnover rate in the first year.5 Employers can help to ensure that new nurses are supported effectively and appropriately in the workplace. To enhance graduates’ transition to practice, many healthcare providers offer transition programs, preceptorships, and workshops.4,6
Led by ANMF (Victorian Branch), the registered undergraduate student employment model was initially trialled by the Victorian Labor Government in 2016 to reduce workload pressure for registered nurses, support transition to practice, and develop a sustainable nursing workforce, and enhance the patient’s experience.7,8,9 The RUSON Employment Model has since been implemented in over 50 Victorian health services and has also led to implementation of an equivalent model for undergraduate midwifery students.
Evaluation of the RUSON Employment Model has yielded promising results. These include reducing workload pressure and increasing job satisfaction for registered nurses, improving patient care, and increasing the confidence of RUSONs in terms of providing general nursing care, teamwork, and communication.7,8

While the RUSON Employment Model is thought to support transition to practice for participants, further research is required to better understand their experiences of the model and factors within the Model which influence its successful implementation. The lead author of this article is a nurse and current PhD student at UniSA undertaking a project to investigate transition to practice in the context of the RUSON Employment Model supervised and supported by the ANMF Federal Office and ANMF Victorian Branch. We hope interested readers will keep a lookout for opportunities to participate in this research which will be announced as they open for recruitment.
Authors
Seung A (Sarah) Park PhD Candidate, University of South Australia, Clinical and Health Sciences, Rosemary Bryant AO Research Centre
Rebecca Sharp PhD, Lecturer, University of South Australia, Clinical and Health Sciences, Rosemary Bryant AO Research Centre
Professor Marion Eckert, Professor, University of South Australia, Clinical and Health Sciences, Rosemary Bryant AO Research Centre
Belinda Clark, Professional Officer, Australian Nursing and Midwifery Federation (ANMF) Victorian Branch
Micah DJ Peters PhD, Senior Research Fellow/National Policy Research Adviser, National Policy Research Unit (Federal Office), Australian Nursing and Midwifery Federation (ANMF) and University of South Australia, Clinical and Health Sciences, Rosemary Bryant AO Research Centre
References
1. World Health Organization. State of the world’s nursing 2020: investing in education, jobs and leadership. Online: WHO. 2021, Available: who.int/publications/i/ item/9789240003279 (Accessed 5 Oct 2022).
2. International Council of Nurses. International Council of Nurses Policy Brief 2021: The global nursing shortage and nurse retention. Online: ICN. Available: icn. ch/sites/default/files/inlinefiles/ICN%20Policy%20Brief_ Nurse%20Shortage%20and%20 Retention_0.pdf (Accessed 5 Oct 2022).
3. Phillips C, Kenny A, Esterman A, Smith C. Does the choice of pre-registration paid employment impact on graduate nurse transition: an Australian study. Nurse Education Today. 2014 Apr 1;34(4):532-7.
4. Cubit KA, Ryan B. Tailoring a graduate nurse program to meet the needs of our next generation nurses. Nurse Education Today. 2011 Jan 1;31(1):65-71.
5. Laschinger HK. Job and career satisfaction and turnover intentions of newly graduated nurses. Journal of Nursing Management. 2012 May;20(4):472-84.
6. Ankers MD, Barton CA, Parry YK. A phenomenological exploration of graduate nurse transition to professional practice within a transition to practice program. Collegian. 2018 Jun 1;25(3):319-25.
7. Kenny A, Dickson-Swift V, DeVecchi N, Phillips C, Hodge B, Masood Y. Evaluation of a rural undergraduate nursing student employment model. Collegian. 2021 Apr 1;28(2):197-205.
8. Mumford S, Newton M, Benzie C, Forster D, Matthews R, Hyde R, Llewelyn F, McLachlan H. Supporting the midwifery workforce: an evaluation of an undergraduate midwifery student employment model at a large tertiary maternity service in Victoria, Australia. Women and Birth. 2022 May 5 [Ahead of Print].
Does the RUSON employment model support transition to practice, relieve workload pressure and improve patient care?
Can paid employment models for undergraduate nurses improve transition to practice and help to address workforce shortages?
FOCUS 52 Jan–Mar 2023 Volume 27, No. 10
Building research capacity through an undergraduate vacation scholarship program
By Casey Marnie, Chantal Hunter, Yi Sun and Micah DJ Peters
Building research capacity and pathways to future higher-degree research is important. This is not only to support the ongoing development of skills necessary to stay up to date with evidence-based practice, but also to build confidence and ability in our early career nurses and midwives.
With limited opportunity for undergraduates to engage in formal research training, we sought to develop an approach that exposed students to a real research environment while allowing them to pursue research into an area of their interest. We advertised two projects within the University of South Australia’s paid vacation research scholarship program and were fortunate to receive two exceptional applicants who displayed a keen willingness to engage with the program.
We sought to create a mentorship experience that allowed the students to develop an idea, follow a research methodology, write for publication, gain experience in searching and critically appraising peer-reviewed literature, and learn the skills and insight necessary to achieve future success in research and evidence-based healthcare.
We worked closely with both students to author and submit research protocols utilising a methodology of their choice and publish articles explaining key findings or concepts in their area of study in ANMJ Online.
Yi Sun, a 3RD year nursing undergraduate, was interested in understanding what aspect of their work Generation Z nurses most valued, hoping to inform organisational policy to attract and retain this emerging workforce. Chantal Hunter, a 2nd-year undergraduate nurse, sought to explore what barriers and enablers exist in providing culturally safe care to gender-diverse people (eg. LGBTIQ+) within emergency departments.
Utilising a two-tier mentorship approach, Dr Micah Peters provided high-level guidance and insight as Yi and Chantal developed their ideas and work. Casey Marnie then provided day to day support and guidance as the students progressed their research. This also included regular discussions around the purpose and conduct of the research, why rigor in research is important, and how research influences policy and practice.
This autonomous approach allowed students to be self-driven, adjusting their review questions and focus as they learnt more about the topics through searching and critical appraisal of the literature. A large part of undertaking research is learning to overcome obstacles in your thinking as you develop and review ideas. By providing a supportive and professional environment, both students engaged in dynamic discussions about their research challenges and insights and maintained momentum as they progressed their research.
In line with the objectives, both successfully published their articles in ANMJ and submitted manuscripts to peer-reviewed journals. The students have also learned how to evaluate and respond to requests for revisions from journals, one of the most harrowing but necessary aspects of publishing good research.
Several factors contributed to this success, the most important of which was flexibility. With Yi completing his nursing degree when the program began and Chantal transitioning from 2ND to 3RD year, both had competing commitments, including placements, transition to practice program participation, and other areas beyond work and study.
Both expressed an appreciation for the respect and trust placed in them to manage and deliver on their research around these commitments.
Yi and Chantal also felt increased confidence in their ability in writing and other research skills, including accessing and analysing information from credible sources. They also found the program allowed them to engage with the research community in their local hospitals. Through this involvement and the skills they had developed, they felt empowered to drive change in their work environments. They felt more confident, had more contacts, and a clear pathway towards future research. Both found the decision to undertake the program was invaluable and one of the best experiences of their undergraduate degrees.
The success of this novel approach to supporting undergraduate research leads us to think about how students interested in research can be supported to overcome hurdles and build the necessary skills to contribute to the development of evidencebased practice early in their careers. The Rosemary Bryant AO Research Centre will continue to support undergraduate nurses and midwives. With the program running again this year, we’re looking forward to meeting and sharing the excitement of research with our new students.
Authors
Casey Marnie and Micah DJ Peters PhD work at the National Policy Research Unit (Federal Office), Australian Nursing and Midwifery Federation (ANMF) and the University of South Australia, Clinical and Health Sciences, Rosemary Bryant AO Research Centre.
Chantal Hunter is a third-year registered nursing student and an inaugural Rosemary Bryant AO Research Centre Summer Research Scholar.
Yi Sun is a registered nurse at St Andrew’s Hospital and an inaugural Rosemary Bryant AO Research Centre Summer Research Scholar

FOCUS Jan–Mar 2023 Volume 27, No. 10 53
Chantal Hunter Yi Sun
Scoping and redesign of the nursing and midwifery clinical facilitator learning support model in northern Queensland
By Lisa Evans
‘Australia is fast approaching a dire nurse shortage’.1 Workforce strategists report a significant reason employees leave organisations is lack of training and development opportunities.2



Considering learning in the workplace is a highly valued enabler of evidence-based care provision and continual improvement,3 and the emerging minimum employee expectations of skill-building and career development opportunities,4 this project’s findings have potential transferability to invigorate nursing and midwifery (N&M) clinical learning support models.
Clinical Facilitators (CFs) are clinical nurses and midwives who provide clinical learning support for the organisation’s N&M clinical staff. CF positions (and roles) vary considerably across the organisation as they have emerged over time aligned to specific unit needs, resulting in inconsistent availability of CF clinical learning support across the organisation.
We took up the challenge to review and detail how current CF learning support models are delivered throughout the organisation and identify redesign opportunities. Undertaken by a project manager with experience and qualifications in clinical redesign and improvement science, incorporating N&M clinicians, CFs, educators, and managers, we undertook a journey to understand the current CF models across the organisation, systems in place, and insights of the N&M workforce. In June-September 2022, a myriad of diagnostics was undertaken, including an online survey for all N&M staff; CF self-report activity diary; focus groups and workshops; and analysis of standard secondary data such as workforce demographics.
Themes that emerged and key diagnostic data, along with root causes identified by our N&M, formed the basis of solution
Innisfail dialysis unit – Sue (CF) and Abbie RN (GNP) – blood volume monitoring
CF Jeff and RN (CDP) Hannah (priming chemotherapy)
FOCUS 54 Jan–Mar 2023 Volume 27, No. 10
CF Loz and RN Shannon Endo-Manometry&ph study
CF-SCOPING SOLUTIONS DESIGN
FUTURE STATE
co-design. Our N&M generated a breadth of innovative solution ideas, which were consolidated into two overarching solutions:
1. Create a CHHHS Clinical Facilitator (CF) model.
2. Establish sustainable CHHHS nursing and midwifery workforce clinical learning support.
Considering the CF role is unique and can create tension, as the individual spans two different worlds –the clinical nurses’ practice world, and the theoretical world of academia,5 the first step to best practice for CFs is meeting role expectations. CHHHS is on track to develop a robust CF model, incorporating CF career pathways, and learning framework that is transparent and available for all CFs. CFs have an essential role in developing a safe and committed N&M workforce, with a key component- the pedagogy in facilitation. Thus, it is vital for CFs evidence-based practice to have focused training, with the theoretical underpinning of feedback for learning and assessment, and peer and mentor support so that ‘craft knowledge’ can be shared.5
Creating sustainable methods to provide N&M clinical learning support is a challenge to be embraced, and CFs, through actively advancing their sub-specialty, are well placed to provide on the ground clinical learning support and enact translation of evidence into practice.5
References
1. Victoria University online. Understanding the nursing shortage in Australia [Internet]. Melbourne VIC: Victoria University; 2022 [updated 2022 Jan 12; cited 2022 Oct 17]. Available from Understanding the nursing shortage in Australia | VU Online
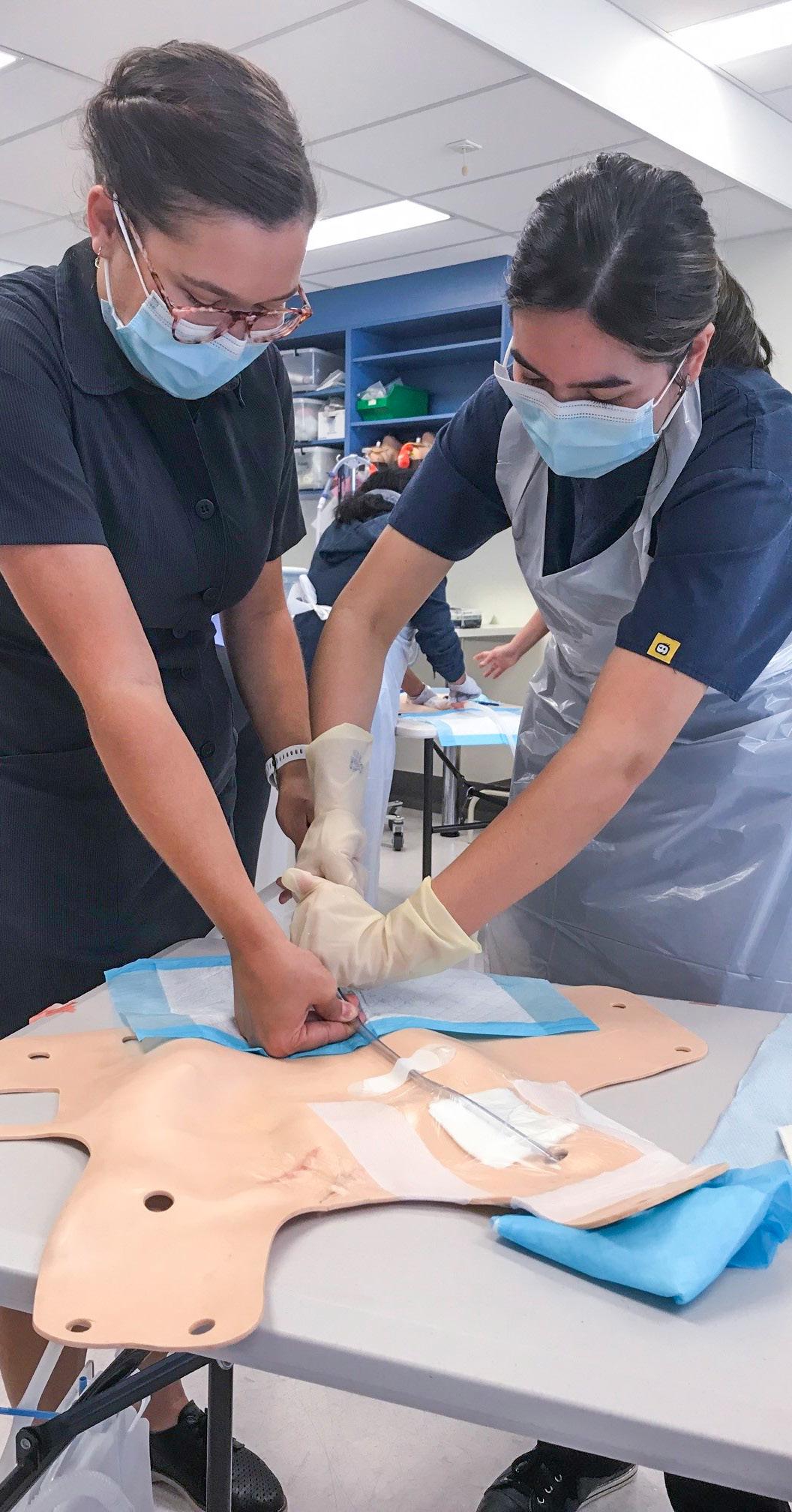
2. Begley P, Dunne L. Turnover and retention report. Melbourne (AU): Australian HR Institute (AU); 2018. 22p.
3. Davis K, White S, Stephenson M. The influence of workplace culture on nurses’ learning experiences: a systematic review of qualitative evidence. JBI Database System Rev Implement Rep 2016 Jun;14(6):274-346. DOI: 10.11124/JBISRIR-2016-002219. PMID: 27532660.
4. Cottier M. Employee expectation gap analysis. Washington (US): Advisory Board; 2022. 2p. Report WF8154436
5. Ryan C, McAllister M. Professional development in clinical facilitation: An integrated review. Collegian [Internet]. 2021 [cited 2022 Oct 17]; 28(1):121-7. Available from DOI 10.1016/j. colegn.2020.02.007
Author Lisa Evans RN, GradCert(Clinical Redesign), GradCertCritCare(Emergency) is Clinical Redesign, CF-Scoping project manager, Cairns and Hinterland Hospital and Health Service in Qld
nursing and midwifery staff have developed solutions to address the diagnostic themes.
CHHHS
OVERARCHING SOLUTIONS DELIVERABLES
1. Create a CHHHS Clinical Facilitator model 2. Establish sustainable nursing and midwifery (N&M) workforce clinical learning support A. CHHHS CF Role Description B. CHHHS CF Business rulesprocesses, performance, reporting C. Model
governance, interactions, services
A. Clinical learning support strategy for further development (solution ideas captured
solutions
tracked) and aligned through HHS N&M strategic plan CURRENT STATE KEY DIAGNOSTIC THEMES 1. Variable CF role and scope. 2 Variable CF career pathway. 3. Value of nursing and midwifery learning 4. Learning support capacity to meet demand
AND OPTIONS
of care (service)-
D. Career pathway and learning framework- training program, mentoring, entry, pathing
from
design workshop
FOCUS Jan–Mar 2023 Volume 27, No. 10 55
CF-Valentina and Catherine-ICC dressing training
Welcome to Healthy Eating
Each issue we will be featuring a recipe from Maggie Beer’s Foundation, which ensures research, education and training will lead to better outcomes and the delivery of nutritious and flavoursome meals to our ageing population in nursing homes. Maggie’s vision is not only to improve nutrition and wellbeing for the aged, but also for all who enjoy good wholesome food.

Peaches stuffed with ginger and almonds

Preparation 15 mins
Cooking 10–20 mins
INGREDIENTS
4 ripe yellow or white peaches
20g toasted flaked almonds
25g finely chopped crystallised ginger
50g unsalted butter, finely diced
2 teaspoons lemon zest
1 teaspoon ground ginger
Pouring cream to serve, optional
METHOD
1. Pre heat a fan forced oven to 200c
2. Halve the fruit and remove the seeds and any bruised flesh, then scoop out a little extra flesh, to make a bigger hollow. (Chop the scooped flesh)
3. Finely chop two-thirds of the almonds, then mix the chopped flesh with chopped almonds, ginger, butter, lemon zest and ground ginger. Combine well to make a paste, then pile it into the cavities in the peach halves.
We invite you to try and make Maggie’s recipes
Send a photo of you and your creation from this issue, and in a sentence, let us know what you liked about It. If we pick your entry, we’ll publish it in the next ANMJ and reward you with a $50 Maggie Beer voucher. Send your entry to: healthyeating@anmf.org.au
Theo Allen, good job on making Maggie’s, potato, leek, lemon and parmesan soup, published last issue. We hope you enjoy your $50 Maggie Beer voucher.

“This potato, leek, lemon and Parmesan soup hit the spot on a Victorian cold turn in November recently. Sharing it with some nursing and midwifery friends last night, it was nourishing, healthy, delicious, and easy to prepare. We all had a very nice evening. (And some left over for work the next day!!!),” says Theo Allan
4. Place on a baking tray lined with baking paper. Bake for 10 minutes or until the fruit is tender and still holding its shape.
5. Scatter with the remaining almonds and serve hot, warm or cold with any juices and a splash of cream, if desired.
HEALTHY EATING 56 Jan–Mar 2023 Volume 27, No. 10
A great way to utilise less than ripe fruit, the roasting process softens the peaches and bring out their perfume and flavour.
Face the future with confidence
At HESTA, we invest time in your super, to help you invest in your future.
Our online Future Planner tool, Retirement Income Stream, and Transition to Retirement Income Stream are just some of the many ways we’re supporting our members to retire with confidence.

Learn more at hesta.com.au
Issued by H.E.S.T. Australia Ltd ABN 66 006 818 695 AFSL 235249, the Trustee of HESTA ABN 64 971 749 321. This information is of a general nature. It does not take into account your objectives, financial situation or specific needs so you should look at your own financial position and requirements before making a decision. You may wish to consult an adviser when doing this. The target market determination for HESTA products can be found at hesta.com.au/tmd Before making a decision about HESTA products you should read the relevant Product Disclosure Statement (call 1800 813 327 or visit hesta.com.au for a copy), and consider any relevant risk (visit the HESTA website for more information).


What will you learn today? With unlimited access to over 650 resources in 20+ practice areas Ausmed makes it even easier to earn your CPD. Scan QR code with your phone Join the 1000s of health professionals and workers learning with Ausmed. Subscribe to Ausmed today Rated 4.7 14.2K Ratings on App Store






































 Image by Lydia Downe
Image by Lydia Downe








 Advanced Practice Nurse Alison Wong, ED Nurse Practitioner Stuart Smith and Palliative Care Nurse Practitioner Juliane Samara lobbying politicians in Canberra last October.
Photo: Lydia Downe
Advanced Practice Nurse Alison Wong, ED Nurse Practitioner Stuart Smith and Palliative Care Nurse Practitioner Juliane Samara lobbying politicians in Canberra last October.
Photo: Lydia Downe
















 By Natalie Dragon
By Natalie Dragon








 By
By





 By Julie Lavery
By Julie Lavery

 By Chiane Marshall
By Chiane Marshall
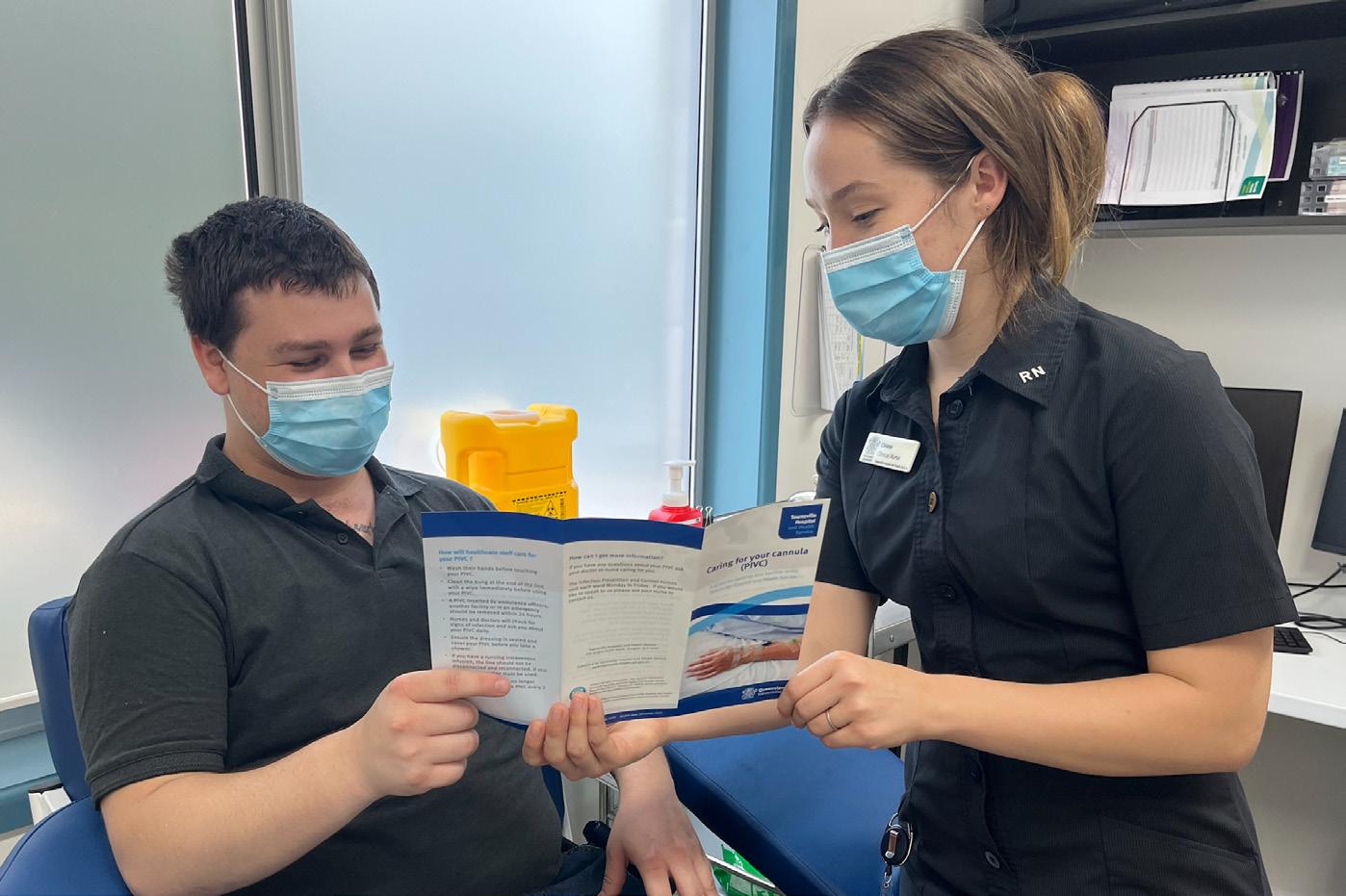
















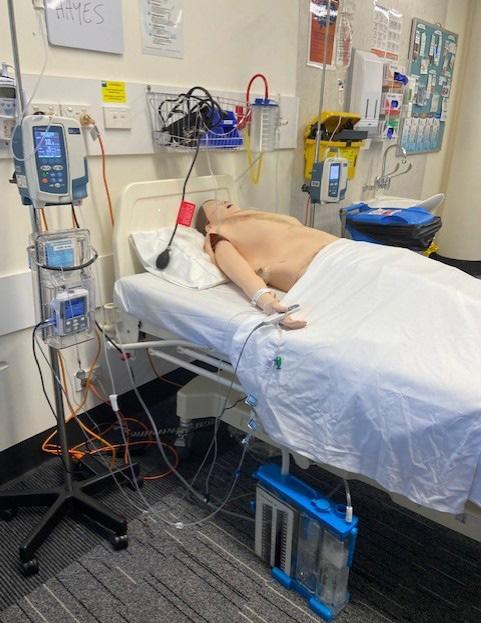 By Sandra Johnston, Lori Delaney, Pauline Gillan, Naomi Tutticci, Karen Theobald and Joanne Ramsbotham
By Sandra Johnston, Lori Delaney, Pauline Gillan, Naomi Tutticci, Karen Theobald and Joanne Ramsbotham