- 1Gastrointestinal Oncology Service, Division of Solid Tumor Oncology, Department of Medicine, Memorial Sloan Kettering Cancer Center, New York, NY, United States
- 2Computer Engineering Program, Columbia University, New York, NY, United States
Esophagogastric cancer (EGC) remains a major cause of cancer-related mortality. Overall survival in the metastatic setting remains poor, with few molecular targeted approaches having been successfully incorporated into routine care to-date: only first line anti-HER2 therapy in ERBB2-expressing tumors, second line anti-VEGFR2 therapy with ramucirumab in unselected patients, and pembrolizumab in PD-L1 expressing or MSI-H patients. EGFR inhibitors were extensively studied in EGC, including phase III trials with cetuximab (EXPAND), panitumumab (REAL3), and gefitinib (COG). All three trials were conducted in unselected populations, and therefore, failed to demonstrate clinical benefit. Here, we review previous attempts at targeting EGFR in EGC and potential future biomarkers for targeting this pathway in patients with EGFR-amplified tumors.
Introduction
Esophagogastric cancer (EGC), consisting of esophagogastric junction adenocarcinoma (EGJ) and distal gastric adenocarcinoma (GC), remains a leading cause of cancer-related mortality (1). In the metastatic setting, median overall survival remains approximately 11 months with optimal palliative chemotherapy in epidermal growth factor receptor 2 (ERRB2) negative patients (2). Molecularly, EGC consists of four distinct subtypes: Epstein Barr Virus-positive (EBV+), microsatellite instability-high (MSI-H), chromosomally unstable (CIN), and genomically stable (GS) (3, 4). While EBV+ and MSI-H tumors have frequent responses to PD-1 inhibition, these represent only ~10–15% of metastatic EGC patients; the vast majority of patients have CIN tumors. CIN tumors characteristically acquire chromosomal instability earlier in their tumorigenesis, which results in copy number amplification of numerous receptor tyrosine kinases, including ERBB2, EGFR, MET, KRAS, and FGFR2 (5–8). Clinical trials of agents targeting these pathways have had mixed results in EGC. However, interpretation of these results requires understanding both the agents used and the study population.
Epidermal growth factor receptor (EGFR or ERBB1) is a 170-kDa transmembrane receptor. While other ERBB family members such as ERBB2 and ERBB3 depend on heterodimer complexes to generate downstream signaling, EGFR binds to multiple ligands, including EGF, which results in homo- and hetero-dimer formation, and subsequent tyrosine phosphorylation of the cytoplasmic domain. Ultimately, EGFR activation triggers a signaling cascade of cell proliferation and survival signaling via activation of MAPK, STAT5, and Ras-Raf-MEK pathways (Figure 1) (9, 10). EGFR-overexpressing EGC tumors are associated with higher stage, more poorly differentiated histology, increased vascular invasion, and potentially shorter survival (11, 12).
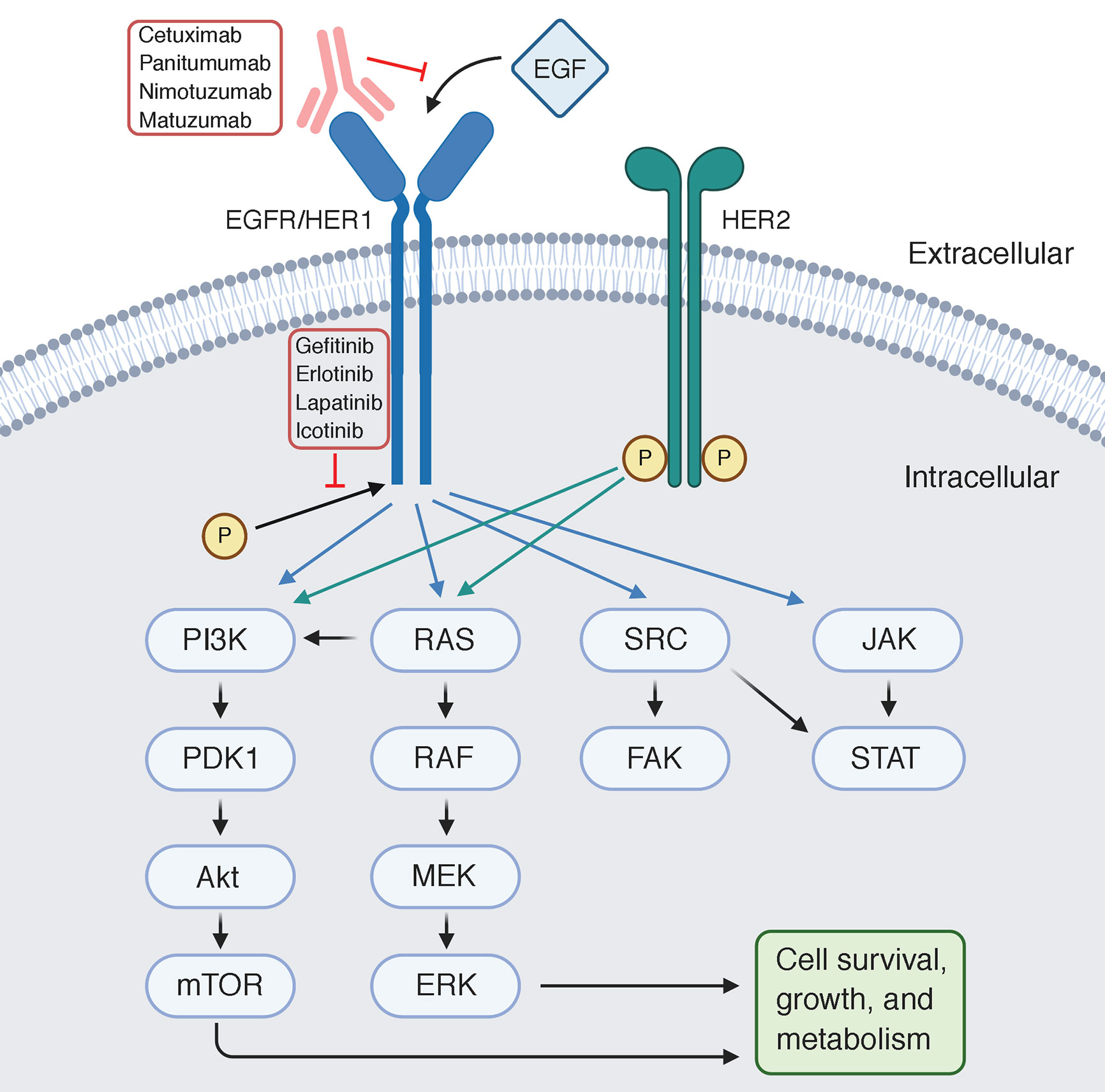
Figure 1 Schematic of EGFR and its downstream pathways with monoclonal antibodies exerting their effects at the extracellular domain, and small molecule inhibitors inhibiting phosphorylation intracellularly.
EGFR is highly expressed in many cancers and amplified in 8.5% of solid tumors, including colorectal cancer (16.3%), non-small cell lung cancer (9%), genitourinary cancers (8.1%), and breast cancer (7.3%) (13). EGFR is also expressed on approximately 30% of EGC tumors and amplified in 6% of patients with metastatic EGC (14–16). Therefore, EGFR-targeting agents entered the clinic in multiple cancer types, with mixed success.
EGFR Therapy Patient Selection
Gefitinib, a small molecule inhibitor of EGFR, entered phase I trials in 1998 and demonstrated a 25% ORR in unselected patients with NSCLC. During phase II trials, responses were more likely in patients with lung adenocarcinoma who were female, never-smokers, and of Asian origin; and it was not until 6 years later that EGFR mutations were published as biomarkers of response to EGFR inhibitors (17). Applying this knowledge, the phase III I-PASS trial selected East Asian patients with lung adenocarcinoma and minimal smoking history and demonstrated that only EGFR-mutated patients benefited from gefitinib (18). In the past decade, this finding has led to approval of gefitinib, erlotinib, afatinib, osimertinib, dacomitinib, and necitumumab in the 15% of patients with EGFR-mutated NSCLC. EGFR inhibition with cetuximab in colorectal cancer underwent a concurrent transformation from benefit across the patient population (19), to those without KRAS mutations (20, 21), and now even more limited to those with left-sided pan-RAS wildtype tumors (22, 23). In both lung and colon adenocarcinomas, efficacy is dependent on patient selection.
Targeting EGFR in Metastatic EGC (mEGC)
Numerous EGFR-targeting phase II studies evaluated cetuximab (24–37), panitumumab (38, 39), nimotuzumab (40, 41), lapatinib (42, 43), erlotinib (44, 45), gefitinib (46), matuzumab (47), and icotinib (48) in mEGC patients (Table 1). As a monotherapy in an unselected population, cetuximab had modest benefit with an ORR of 5% and a median progression-free survival (mPFS) of 4.0 months in these patients—including one patient with an 11.3 month PFS—which suggested that a small subset of patients benefits from EGFR-directed therapy (36). Subsequent evaluation with gefitinib in EGFR-expressing (46), and erlotinib+radiation or icotinib in EGFR-amplified patients (45, 48) further supported this premise.
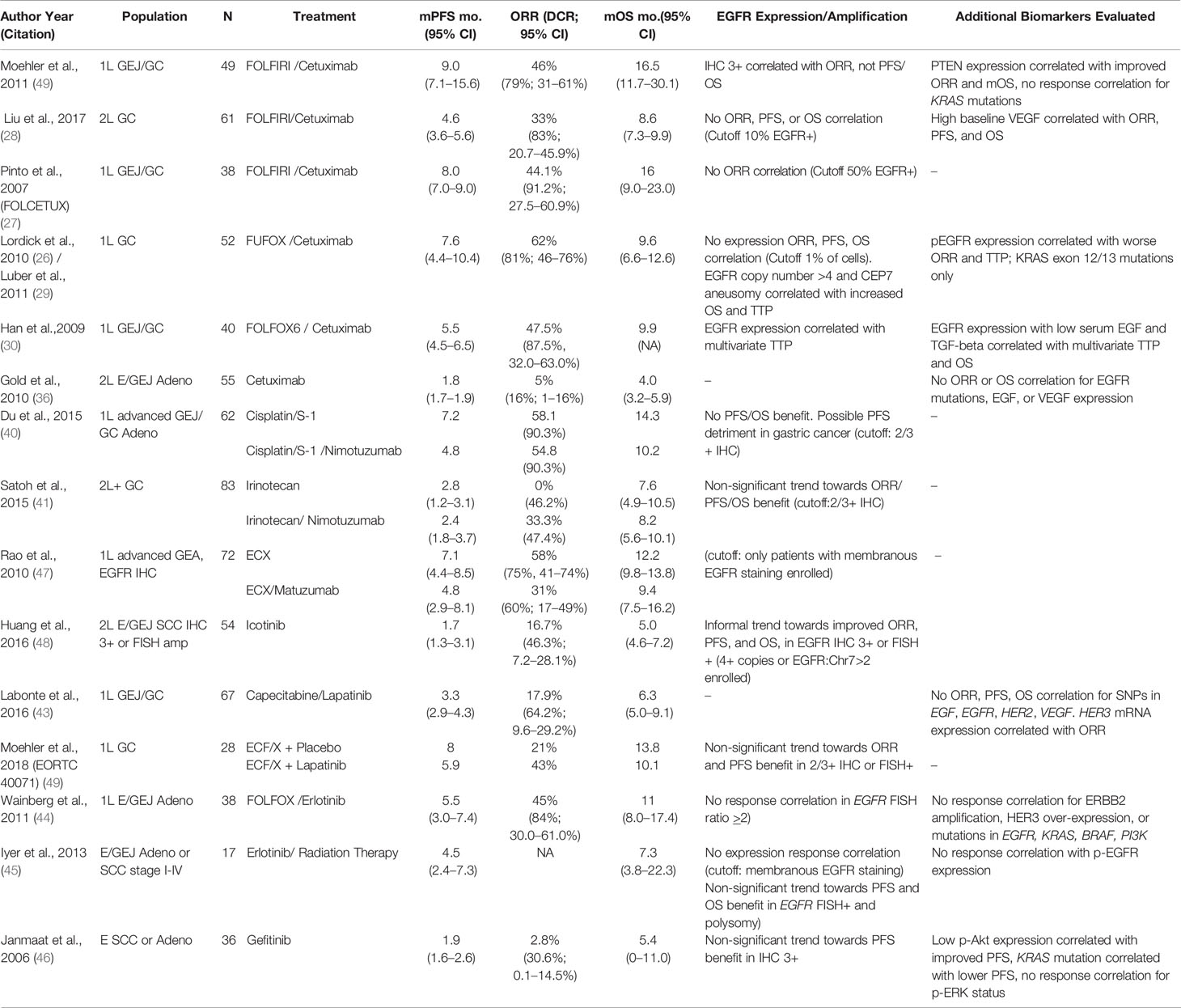
Table 1 Phase II mEGC trials evaluating EGFR inhibitors evaluating predictive and/or prognostic biomarkers.
Countless combinations of EGFR inhibitors with chemotherapy demonstrated mixed results. Whereas some demonstrated mPFS exceeding 8 months (48, 49), others suggested that adding EGFR inhibitors may even be detrimental (40). Biomarker analyses sought to delineate a sub-population that benefited from EGFR inhibition, but utilized inadequate and inconsistent expression and copy number definitions. In biomarker analyses, EGFR expression demonstrated mixed results. Many studies defined low EGFR expression cutoffs, and therefore failed to identify a correlation with response and survival (25, 26, 28, 40, 45, 47), which mirrors the lack of trastuzumab benefit in ERBB2 low-expressors in ToGA (50). However, response and survival benefits were suggested in nearly all studies that used more clinically relevant cutoffs of IHC 2/3+ (30, 41, 42, 46, 48, 49) or gene amplification (29, 42, 45, 48) (Table 1). One study indicated that VEGF expression may be prognostic for response to therapy (28), as might EGFR expression in conjunction with EGFR amplification or low EGF expression (30). Patients with gastroesophageal junction tumors demonstrating increased EGFR gene copy number or expression may also derive more benefit than those with gastric primary tumors (29, 40). These findings are all limited by small sample size, inconsistent definitions of EGFR-expression and amplification, tumor heterogeneity, and patient population.
In colorectal cancer, absence of RAS mutations and sidedness were found to be better predictors of response than EGFR expression or amplification (21, 51). However, activating mutations in RAS and BRAF are less commonly found in EGC, and so no correlation was seen between KRAS, BRAF, or PIK3CA mutations and survival in mEGC trials (26, 49). All of these correlative biomarkers were evaluated in small phase II studies—mostly single arm in unselected patients—and utilized inconsistent expression and copy number cutoffs. Consequently, these studies were insufficiently powered to identify a predictive biomarker. Therefore, subsequent phase III trials proceeded in unselected populations.
Based upon these findings, first-line phase III trials of chemotherapy in combination with cetuximab (EXPAND) and panitumumab (REAL3) were conducted in patients with esophagogastric cancer (52, 53) (Table 2). In EXPAND, 904 first-line advanced EGC patients were randomized to receive 3-week cycles of twice daily capecitabine 1,000 mg/m2 on days 1–14 and IV cisplatin 80 mg/m2 with or without cetuximab 400 mg/m2 on day 1 followed by 250 mg/m2 weekly with a PFS primary endpoint. Addition of cetuximab failed to improve mPFS (4.4 months with cetuximab vs 5.6 months without; HR 1.09; 95% CI 0.92–1.29; p = 0.32) and median overall survival (mOS) (9.4 months with cetuximab vs 10.7 months without; HR 1.00; 95% CI 0.87–1.17; p = 0.95). EGFR IHC was evaluated as a predictive biomarker, and most patients exhibited little to no staining. However, amongst patients with the top 6% of EGFR expression, there was a trend towards improved mPFS (HR 0.62; 95% CI 0.28–1.35) and mOS (HR 0.68; 95% CI 0.34–1.39), whereas no beneficial trend was seen in patients with less EGFR expression (54). These findings suggest that there may be a select population that benefits from cetuximab, though too small to be effectively studied in an unselected population. A similar issue was seen in REAL3.
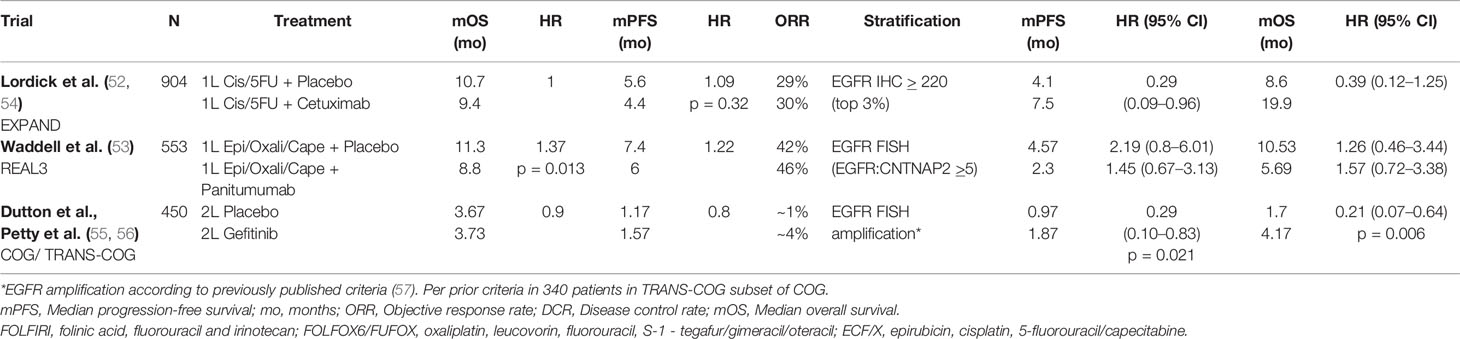
Table 2 Phase III mEGC trials evaluating EGFR inhibitors including subset analysis by EGFR expression or EGFR amplification.
In REAL3, 553 untreated advanced EGC patients were randomized to receive day 1 IV epirubicin 50 mg/m2, day 1 IV oxaliplatin 130 mg/m2, and daily capecitabine 1,250 mg/m2 (ECX) with or without panitumumab 9 mg/kg on day 1 of a 3-week cycle with a primary endpoint of OS (53). Accrual was terminated after interim analysis revealed that patients who received ECX and panitumumab had a significantly shorter mOS of 8.8 vs 11.3 months (HR 1.37, 95% CI 1.07–1.76, p = 0.013) than patients who did not receive panitumumab (53). Patients with EGFR-amplified tumors trended non-significantly towards having inferior progression-free and overall survival, regardless of treatment arm, suggesting that EGFR amplification portends a worse prognosis. Even in patients with tissue or plasma ddPCR EGFR:CNTNAP2 copy number ratio >2 (6.2%) or >5 (2.7%), the addition of panitumumab failed to prolong progression-free and overall survival (58). One explanation is that these disappointing results reflect an interaction between panitumumab and an epirubicin-containing chemotherapy regimen, as all phase 2 and 3 mEG trials adding EGFR inhibition to an anthracycline triplet trended towards inferior survival (38, 42, 47, 53). In fact, in its initial form, the REAL3 regimen caused unacceptable toxicity, and therefore required an unplanned formal dose-finding study leading to a modified regimen in which oxaliplatin was reduced from 130 mg/m2 to 100 mg/m2 and capecitabine from 1,250 mg/m2 to 1,000 mg/m2/d. However, reduced dose-intensity may also account for inferior clinical outcomes. Therefore, no further evaluation of panitumumab has been performed.
While EXPAND and REAL3 evaluated EGFR inhibition in the first-line, COG assessed second-line gefitinib versus placebo in 449 unselected esophageal/GEJ adenocarcinoma or squamous cell carcinoma patients (55). Once again, COG failed to achieve its primary endpoint. Gefitinib demonstrated a modest mPFS benefit versus placebo (1.57 vs 1.17 months, HR 0.80, 95% CI 0.66–0.96) without an overall survival benefit (3.73 vs 3.67 months, HR 0.90, 95% CI 0.74–1.09) in unselected patients. However, 3% of gefitinib-treated patients achieved a partial response—lasting up to 7.33 months. TRANSCOG evaluated molecular correlations in tissue from patients enrolled in COG, including mutations in EGFR, PIK3CA, BRAF, and KRAS as well as copy number gain (38/292 patients) or EGFR amplification by FISH (21/292 patients) (56). While no differences were seen when stratifying by gene mutation status, patients with EGFR FISH+ tumors (either copy-number gain or amplification) derived a mPFS benefit (HR 0.42, 95% CI 0.22–0.81, p = 0.01) but not a mOS benefit (HR 0.57, 95% CI 0.30–1.06, p = 0.08) from gefitinib versus placebo in multivariate analysis. Most notably, the 21/292 (7.1%) patients with EGFR-amplified tumors achieved both a PFS and OS benefit with the addition of gefitinib, with a mPFS of 1.87 vs 0.97 months (HR 0.29, 95% CI 0.10–0.83, p = 0.021) and mOS 4.17 vs 1.70 months (HR 0.21, 95% CI 0.07–0.64, p = 0.006). Thus, the degree of EGFR amplification appears to predict EGFR inhibitor activity in mEGC.
Based upon these findings, a small cohort of patients with EGFR-amplified mEGC was treated with EGFR inhibitors. Patients received first-line FOLFOX+Abt-806, second-line FOLFIRI+cetuximab, or third or greater line cetuximab monotherapy. In this heterogeneous, though selected, population, 57% of patients achieved an objective response rate (ORR) with a mPFS of 10 months—including 14 months in a patient receiving cetuximab monotherapy (16, 59). Though the cohort was small and heterogeneous, these findings are consistent with the phase III subset analyses from EXPAND and TRANS-COG. As seen in ERBB2-targeting trials, this study also demonstrated resistance mechanisms to EGFR-directed therapies—namely selection of RAS, PIK3CA, and ERBB2 altered and non-EGFR-amplified clones. Thus, tumor heterogeneity adds yet another layer of complexity to patient selection for targeted therapies in mEGC.
Novel Approaches Targeting EGFR
Receptor tyrosine kinase blockade prolongs progression-free and even overall survival in many populations, but is limited by intratumoral heterogeneity and upregulation/activation of redundant or downstream signaling. Outside of mEGC, newer investigational agents attempt to deliver targeted cytotoxic payloads or prime an immune-mediated response.
Phase 1 data for MRG003, a fully human anti-EGFR IgG1 antibody conjugated to monomethyl auristatin E stabilized disease in an EGFR-expressing esophageal cancer patient that remains on treatment at 12 weeks (57). A similar phase I dose-escalation study of ABBV-321 (serclutamab talirine), an antibody-drug conjugate combining a humanized immunoglobulin G1 anti-EGFR antibody conjugated to a pyrrolobenzodiazepine dimer, remains underway in EGFR-over-expressing patients (NCT03234712) (60). One novel approach, EDV-D682, contains a bacterially derived EDV nanocell loaded with PNU-159682, a cytotoxic agent, and then coated with an EGFR antibody. In a recent phase 1 pancreatic cancer trial, EDV-D682 achieved radiographic disease control in 8/9 patients, including response in 4/5 evaluable patients, at 4 months. A phase 2 study is currently enrolling patients (ACTRN12619000385145) (61).
Another recent approach utilizes bispecific antibodies that recognize two distinct epitopes. One such agent, amivantamab, is a fully human anti-EGFR and c-MET-targeting antibody that demonstrated a 36% objective response rate and 10 month median response duration in patients with non-small cell lung cancers (NSCLC) harboring EGFR exon 20 insertions (62). The intent of this agent is to co-inhibit MET, which is a common resistance mechanism in EGFR-targeted NSCLC.
Rather than injecting antibodies, another EGFR-targeting approach undergoing investigation in pancreatic cancer collects autologous lymphocytes and expands them in vitro in the presence of OKT3 (anti-CD3) and cetuximab (anti-EGFR) in order to generate bispecific antibody armed T cells (BATs), which are then infused. Of “evaluable” patients in this seven patient phase 1/2 study, the median overall survival was 31 months despite lack of objective radiographic responses, with suggestion of an innate immune response, and better than expected responses to subsequent chemotherapy (63). A second line phase IB study is underway (NCT04137536) in order to confirm these findings.
In a similar manner, a phase 1 study of EGFR-targeted chimeric antigen receptor T-cells (CAR-T) was conducted in China, which demonstrated objective response in 2/11 and disease control in 7/11 patients, though survival data was immature at the time of publication (64). In addition to numerous ongoing EGFR CAR-T trials in China, pediatric evaluation of a second-generation agent targeting both 4-1BB and EGFR is underway in the United States (NCT03618381).
Future Directions
Although all three phase III trials evaluating EGFR inhibition in mEGC failed to achieve their primary endpoints, EGFR biomarker analysis suggests that as in lung and colon cancers, EGFR inhibition has a significant role in a properly selected population. Retrospective analysis of targeting EGFR in EGFR-amplified mEGC patients by tissue and/or circulating tumor DNA next generation sequencing (8, 13), as well as prospective treatment with EGFR inhibitors, suggest that this may represent the ideal population for EGFR inhibition in future EGFR-targeting mEGC studies (16). However, investigators will need to ensure adequate definitions for positivity, as well as pre-specified stratification for baseline resistance mechanisms. Novel compounds including anti-EGFR antibody drug conjugates, bispecific antibodies, and cellular therapies may have a role in overcoming resistance mechanisms. Despite these limitations, six percent of the over one million EGC patients diagnosed each year represents a large patient population needing effective therapies, and so EGFR-targeted therapies merit re-evaluation.
Author Contributions
All authors contributed to the article and approved the submitted version.
Conflict of Interest
SM has received research support from Genentech and travel expenses from Merck and Bayer. YJ has received research funding from Boehringer Ingelheim, Bayer, Genentech/Roche, Bristol-Myers Squibb, Eli Lilly, and Merck and served on advisory boards for Merck Serono, Bristol-Myers Squibb, Eli Lilly, Pfizer, Bayer, Imugene, Merck, Daiichi-Sankyo, and AstraZeneca.
The remaining author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We acknowledge our patients who face this challenging disease. Figure created with BioRender.com
References
1. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin (2018) 68:394–424. doi: 10.3322/caac.21492
2. Wilke H, Muro K, Van Cutsem E, Oh S-C, Bodoky G, Shimada Y, et al. Ramucirumab plus paclitaxel versus placebo plus paclitaxel in patients with previously treated advanced gastric or gastro-oesophageal junction adenocarcinoma (RAINBOW): a double-blind, randomised phase 3 trial. Lancet Oncol (2014) 15:1224–35. doi: 10.1016/S1470-2045(14)70420-6
3. Cancer Genome Atlas Research Network, Analysis Working Group, Asan University, BC Cancer Agency, Brigham and Women’s Hospital, Broad Institute, Brown University, Case Western Reserve University, Dana-Farber Cancer Institute, Duke University, et al. Integrated genomic characterization of oesophageal carcinoma. Nature (2017) 541:169–75. doi: 10.1038/nature20805
4. Cancer Genome Atlas Research Network. Comprehensive molecular characterization of gastric adenocarcinoma. Nature (2014) 513:202–9. doi: 10.1038/nature13480
5. Stachler MD, Taylor-Weiner A, Peng S, McKenna A, Agoston AT, Odze RD, et al. Paired exome analysis of Barrett’s esophagus and adenocarcinoma. Nat Genet (2015) 47:1047–55. doi: 10.1038/ng.3343
6. Zang ZJ, Ong CK, Cutcutache I, Yu W, Zhang SL, Huang D, et al. Genetic and structural variation in the gastric cancer kinome revealed through targeted deep sequencing. Cancer Res (2011) 71:29–39. doi: 10.1158/0008-5472.CAN-10-1749
7. Deng N, Goh LK, Wang H, Das K, Tao J, Tan IB, et al. A comprehensive survey of genomic alterations in gastric cancer reveals systematic patterns of molecular exclusivity and co-occurrence among distinct therapeutic targets. Gut (2012) 61:673–84. doi: 10.1136/gutjnl-2011-301839
8. Maron SB, Chase LM, Lomnicki S, Kochanny S, Moore KL, Joshi SS, et al. Circulating tumor DNA sequencing analysis of gastroesophageal adenocarcinoma. Clin Cancer Res (2019) 25:7098–112. doi: 10.1158/1078-0432.CCR-19-1704
9. Yano S, Kondo K, Yamaguchi M, Richmond G, Hutchison M, Wakeling A, et al. Distribution and function of EGFR in human tissue and the effect of EGFR tyrosine kinase inhibition. Anticancer Res (2003) 23:3639–50.
10. Schulze WX, Deng L, Mann M. Phosphotyrosine interactome of the ErbB-receptor kinase family. Mol Syst Biol (2005) 1:2005.0008. doi: 10.1038/msb4100012
11. Terashima M, Kitada K, Ochiai A, Ichikawa W, Kurahashi I, Sakuramoto S, et al. Impact of expression of human epidermal growth factor receptors EGFR and ERBB2 on survival in stage II/III gastric cancer. Clin Cancer Res (2012) 18:5992–6000. doi: 10.1158/1078-0432.CCR-12-1318
12. Nagatsuma AK, Aizawa M, Kuwata T, Doi T, Ohtsu A, Fujii H, et al. Expression profiles of HER2, EGFR, MET and FGFR2 in a large cohort of patients with gastric adenocarcinoma. Gastric Cancer (2015) 18:227–38. doi: 10.1007/s10120-014-0360-4
13. Kato S, Okamura R, Mareboina M, Lee S, Goodman A, Patel SP, et al. Revisiting Epidermal Growth Factor Receptor (EGFR) Amplification as a Target for Anti-EGFR Therapy: Analysis of Cell-Free Circulating Tumor DNA in Patients With Advanced Malignancies. JCO Precis Oncol (2019) 3:1–14. doi: 10.1200/PO.18.00180
14. Kim MA, Lee HS, Lee HE, Jeon YK, Yang HK, Kim WH. EGFR in gastric carcinomas: prognostic significance of protein overexpression and high gene copy number. Histopathology (2008) 52:738–46. doi: 10.1111/j.1365-2559.2008.03021.x
15. Wang KL, Wu T-T, Choi IS, Wang H, Resetkova E, Correa AM, et al. Expression of epidermal growth factor receptor in esophageal and esophagogastric junction adenocarcinomas: association with poor outcome. Cancer (2007) 109:658–67. doi: 10.1002/cncr.22445
16. Maron SB, Alpert L, Kwak HA, Lomnicki S, Chase L, Xu D, et al. Targeted Therapies for Targeted Populations: Anti-EGFR Treatment for EGFR-Amplified Gastroesophageal Adenocarcinoma. Cancer Discovery (2018) 8:696–713. doi: 10.1158/2159-8290.CD-17-1260
17. Lynch TJ, Bell DW, Sordella R, Gurubhagavatula S, Okimoto RA, Brannigan BW, et al. Activating mutations in the epidermal growth factor receptor underlying responsiveness of non-small-cell lung cancer to gefitinib. N Engl J Med (2004) 350:2129–39. doi: 10.1056/NEJMoa040938
18. Mok TS, Wu Y-L, Thongprasert S, Yang C-H, Chu D-T, Saijo N, et al. Gefitinib or carboplatin-paclitaxel in pulmonary adenocarcinoma. N Engl J Med (2009) 361:947–57. doi: 10.1056/NEJMoa0810699
19. Cunningham D, Humblet Y, Siena S, Khayat D, Bleiberg H, Santoro A, et al. Cetuximab monotherapy and cetuximab plus irinotecan in irinotecan-refractory metastatic colorectal cancer. N Engl J Med (2004) 351:337–45. doi: 10.1056/NEJMoa033025
20. Tournigand C, André T, Achille E, Lledo G, Flesh M, Mery-Mignard D, et al. FOLFIRI followed by FOLFOX6 or the reverse sequence in advanced colorectal cancer: a randomized GERCOR study. J Clin Oncol (2004) 22:229–37. doi: 10.1200/JCO.2004.05.113
21. Van Cutsem E, Köhne C-H, Hitre E, Zaluski J, Chang Chien C-R, Makhson A, et al. Cetuximab and chemotherapy as initial treatment for metastatic colorectal cancer. N Engl J Med (2009) 360:1408–17. doi: 10.1056/NEJMoa0805019
22. Stintzing S, Modest DP, Rossius L, Lerch MM, von Weikersthal LF, Decker T, et al. FOLFIRI plus cetuximab versus FOLFIRI plus bevacizumab for metastatic colorectal cancer (FIRE-3): a post-hoc analysis of tumour dynamics in the final RAS wild-type subgroup of this randomised open-label phase 3 trial. Lancet Oncol (2016) 17:1426–34. doi: 10.1016/S1470-2045(16)30269-8
23. Tejpar S, Stintzing S, Ciardiello F, Tabernero J, Van Cutsem E, Beier F, et al. Prognostic and Predictive Relevance of Primary Tumor Location in Patients With RAS Wild-Type Metastatic Colorectal Cancer: Retrospective Analyses of the CRYSTAL and FIRE-3 Trials. JAMA Oncol (2017) 3:194–201. doi: 10.1001/jamaoncol.2016.3797
24. Enzinger PC, Burtness BA, Niedzwiecki D, Ye X, Douglas K, Ilson DH, et al. CALGB 80403 (Alliance)/E1206: A randomized phase II study of three chemotherapy regimens plus cetuximab in metastatic esophageal and gastroesophageal junction cancers. J Clin Oncol (2016) 34:2736–42. doi: 10.1200/JCO.2015.65.5092
25. Pinto C, Di Fabio F, Barone C, Siena S, Falcone A, Cascinu S, et al. Phase II study of cetuximab in combination with cisplatin and docetaxel in patients with untreated advanced gastric or gastro-oesophageal junction adenocarcinoma (DOCETUX study). Br J Cancer (2009) 101:1261–8. doi: 10.1038/sj.bjc.6605319
26. Lordick F, Luber B, Lorenzen S, Hegewisch-Becker S, Folprecht G, Wöll E, et al. Cetuximab plus oxaliplatin/leucovorin/5-fluorouracil in first-line metastatic gastric cancer: a phase II study of the Arbeitsgemeinschaft Internistische Onkologie (AIO). Br J Cancer (2010) 102:500–5. doi: 10.1038/sj.bjc.6605521
27. Pinto C, Di Fabio F, Siena S, Cascinu S, Rojas Llimpe FL, Ceccarelli C, et al. Phase II study of cetuximab in combination with FOLFIRI in patients with untreated advanced gastric or gastroesophageal junction adenocarcinoma (FOLCETUX study). Ann Oncol (2007) 18:510–7. doi: 10.1093/annonc/mdl459
28. Liu X, Guo W, Zhang W, Yin J, Zhang J, Zhu X, et al. A multi-center phase II study and biomarker analysis of combined cetuximab and modified FOLFIRI as second-line treatment in patients with metastatic gastric cancer. BMC Cancer (2017) 17:188. doi: 10.1186/s12885-017-3174-z
29. Luber B, Deplazes J, Keller G, Walch A, Rauser S, Eichmann M, et al. Biomarker analysis of cetuximab plus oxaliplatin/leucovorin/5-fluorouracil in first-line metastatic gastric and oesophago-gastric junction cancer: results from a phase II trial of the Arbeitsgemeinschaft Internistische Onkologie (AIO). BMC Cancer (2011) 11:509. doi: 10.1186/1471-2407-11-509
30. Han SW, Oh DY, Im SA, Park SR, Lee KW, Song HS, et al. Phase II study and biomarker analysis of cetuximab combined with modified FOLFOX6 in advanced gastric cancer. Br J Cancer (2009) 100:298–304. doi: 10.1038/sj.bjc.6604861
31. Schønnemann KR, Yilmaz M, Bjerregaard JK, Nielsen KM, Pfeiffer P. Phase II study of biweekly cetuximab in combination with irinotecan as second-line treatment in patients with platinum-resistant gastro-oesophageal cancer. Eur J Cancer (2012) 48:510–7. doi: 10.1016/j.ejca.2011.12.005
32. Janjigian YY, Ku GY, Campbell JC, Shah MA, Capanu M, Kelsen DP, et al. Phase II trial of cetuximab plus cisplatin and irinotecan in patients with cisplatin and irinotecan-refractory metastatic esophagogastric cancer. Am J Clin Oncol (2014) 37:126–30. doi: 10.1097/COC.0b013e318271b14f
33. Lorenzen S, Schuster T, Porschen R, Al-Batran SE, Hofheinz R, Thuss-Patience P, et al. Cetuximab plus cisplatin-5-fluorouracil versus cisplatin-5-fluorouracil alone in first-line metastatic squamous cell carcinoma of the esophagus: a randomized phase II study of the Arbeitsgemeinschaft Internistische Onkologie. Ann Oncol (2009) 20:1667–73. doi: 10.1093/annonc/mdp069
34. Wöll E, Greil R, Eisterer W, Bechter O, Fridrik MA, Grünberger B, et al. Oxaliplatin, irinotecan and cetuximab in advanced gastric cancer. A multicenter phase II trial (Gastric-2) of the Arbeitsgemeinschaft Medikamentose Tumortherapie (AGMT). Anticancer Res (2011) 31:4439–43.
35. Richards D, Kocs DM, Spira AI, David McCollum A, Diab S, Hecker LI, et al. Results of docetaxel plus oxaliplatin (DOCOX) ± cetuximab in patients with metastatic gastric and/or gastroesophageal junction adenocarcinoma: results of a randomised Phase 2 study. Eur J Cancer (2013) 49:2823–31. doi: 10.1016/j.ejca.2013.04.022
36. Gold PJ, Goldman B, Iqbal S, Leichman LP, Zhang W, Lenz H-J, et al. Cetuximab as second-line therapy in patients with metastatic esophageal adenocarcinoma: a phase II Southwest Oncology Group Study (S0415). J Thorac Oncol (2010) 5:1472–6. doi: 10.1097/JTO.0b013e3181e77a92
37. Chan JA, Blaszkowsky LS, Enzinger PC, Ryan DP, Abrams TA, Zhu AX, et al. A multicenter phase II trial of single-agent cetuximab in advanced esophageal and gastric adenocarcinoma. Ann Oncol (2011) 22:1367–73. doi: 10.1093/annonc/mdq604
38. Tebbutt NC, Price TJ, Ferraro DA, Wong N, Veillard A-S, Hall M, et al. Panitumumab added to docetaxel, cisplatin and fluoropyrimidine in oesophagogastric cancer: ATTAX3 phase II trial. Br J Cancer (2016) 114:505–9. doi: 10.1038/bjc.2015.440
39. Yoon H, Karapetyan L, Choudhary A, Kosozi R, Bali GS, Zaidi AH, et al. Phase II Study of Irinotecan Plus Panitumumab as Second-Line Therapy for Patients with Advanced Esophageal Adenocarcinoma. Oncologist (2018) 23:1004–e102. doi: 10.1634/theoncologist.2017-0657
40. Du F, Zheng Z, Shi S, Jiang Z, Qu T, Yuan X, et al. S-1 and Cisplatin With or Without Nimotuzumab for Patients With Untreated Unresectable or Metastatic Gastric Cancer: A Randomized, Open-Label Phase 2 Trial. Medicine (2015) 94:e958. doi: 10.1097/MD.0000000000000958
41. Satoh T, Lee KH, Rha SY, Sasaki Y, Park SH, Komatsu Y, et al. Randomized phase II trial of nimotuzumab plus irinotecan versus irinotecan alone as second-line therapy for patients with advanced gastric cancer. Gastric Cancer (2015) 18:824–32. doi: 10.1007/s10120-014-0420-9
42. Moehler M, Schad A, Maderer A, Atasoy A, Mauer ME, Caballero C, et al. Lapatinib with ECF/X in the first-line treatment of metastatic gastric cancer according to HER2neu and EGFR status: a randomized placebo-controlled phase II study (EORTC 40071). Cancer Chemother Pharmacol (2018) 82:733–9. doi: 10.1007/s00280-018-3667-8
43. LaBonte MJ, Yang D, Zhang W, Wilson PM, Nagarwala YM, Koch KM, et al. A Phase II Biomarker-Embedded Study of Lapatinib plus Capecitabine as First-line Therapy in Patients with Advanced or Metastatic Gastric Cancer. Mol Cancer Ther (2016) 15:2251–8. doi: 10.1158/1535-7163.MCT-15-0908
44. Wainberg ZA, Lin LS, DiCarlo B, Dao KM, Patel R, Park DJ, et al. Phase II trial of modified FOLFOX6 and erlotinib in patients with metastatic or advanced adenocarcinoma of the oesophagus and gastro-oesophageal junction. Br J Cancer (2011) 105:760–5. doi: 10.1038/bjc.2011.280
45. Iyer R, Chhatrala R, Shefter T, Yang G, Malhotra U, Tan W, et al. Erlotinib and radiation therapy for elderly patients with esophageal cancer - clinical and correlative results from a prospective multicenter phase 2 trial. Oncology (2013) 85:53–8. doi: 10.1159/000351617
46. Janmaat ML, Gallegos-Ruiz MI, Rodriguez JA, Meijer GA, Vervenne WL, Richel DJ, et al. Predictive factors for outcome in a phase II study of gefitinib in second-line treatment of advanced esophageal cancer patients. J Clin Oncol (2006) 24:1612–9. doi: 10.1200/JCO.2005.03.4900
47. Rao S, Starling N, Cunningham D, Sumpter K, Gilligan D, Ruhstaller T, et al. Matuzumab plus epirubicin, cisplatin and capecitabine (ECX) compared with epirubicin, cisplatin and capecitabine alone as first-line treatment in patients with advanced oesophago-gastric cancer: a randomised, multicentre open-label phase II study. Ann Oncol (2010) 21:2213–9. doi: 10.1093/annonc/mdq247
48. Huang J, Fan Q, Lu P, Ying J, Ma C, Liu W, et al. Icotinib in Patients with Pretreated Advanced Esophageal Squamous Cell Carcinoma with EGFR Overexpression or EGFR Gene Amplification: A Single-Arm, Multicenter Phase 2 Study. J Thorac Oncol (2016) 11:910–7. doi: 10.1016/j.jtho.2016.02.020
49. Moehler M, Mueller A, Trarbach T, Lordick F, Seufferlein T, Kubicka S, et al. Cetuximab with irinotecan, folinic acid and 5-fluorouracil as first-line treatment in advanced gastroesophageal cancer: a prospective multi-center biomarker-oriented phase II study. Ann Oncol (2011) 22:1358–66. doi: 10.1093/annonc/mdq591
50. Bang Y-J, Van Cutsem E, Feyereislova A, Chung HC, Shen L, Sawaki A, et al. Trastuzumab in combination with chemotherapy versus chemotherapy alone for treatment of HER2-positive advanced gastric or gastro-oesophageal junction cancer (ToGA): a phase 3, open-label, randomised controlled trial. Lancet (2010) 376:687–97. doi: 10.1016/S0140-6736(10)61121-X
51. Douillard JY, Siena S, Cassidy J, Tabernero J, Burkes R, Barugel M, et al. Final results from PRIME: randomized phase III study of panitumumab with FOLFOX4 for first-line treatment of metastatic colorectal cancer. Ann Oncol (2014) 25:1346–55. doi: 10.1093/annonc/mdu141
52. Lordick F, Kang Y-K, Chung H-C, Salman P, Oh SC, Bodoky G, et al. Capecitabine and cisplatin with or without cetuximab for patients with previously untreated advanced gastric cancer (EXPAND): a randomised, open-label phase 3 trial. Lancet Oncol (2013) 14:490–9. doi: 10.1016/S1470-2045(13)70102-5
53. Waddell T, Chau I, Cunningham D, Gonzalez D, Okines AFC, Okines C, et al. Epirubicin, oxaliplatin, and capecitabine with or without panitumumab for patients with previously untreated advanced oesophagogastric cancer (REAL3): a randomised, open-label phase 3 trial. Lancet Oncol (2013) 14:481–9. doi: 10.1016/S1470-2045(13)70096-2
54. Lordick F, Kang Y-K, Salman P, Oh SC, Bodoky G, Kurteva GP, et al. Clinical outcome according to tumor HER2 status and EGFR expression in advanced gastric cancer patients from the EXPAND study. J Clin Oncol (2013) 4021. doi: 10.1200/jco.2013.31.15_suppl.4021
55. Dutton SJ, Ferry DR, Blazeby JM, Abbas H, Dahle-Smith A, Mansoor W, et al. Gefitinib for oesophageal cancer progressing after chemotherapy (COG): a phase 3, multicentre, double-blind, placebo-controlled randomised trial. Lancet Oncol (2014) 15:894–904. doi: 10.1016/S1470-2045(14)70024-5
56. Petty RD, Dahle-Smith A, Stevenson DAJ, Osborne A, Massie D, Clark C, et al. Gefitinib and EGFR gene copy number aberrations in esophageal cancer. J Clin Oncol (2017) 35:2279–87. doi: 10.1200/JCO.2016.70.3934
57. Xu R, Qiu M-Z, Zhang Y, Wei X-L, Hu C. First-in-human dose-escalation study of anti-EGFR ADC MRG003 in patients with relapsed/refractory solid tumors. JCO (2020) 38:3550–0. doi: 10.1200/JCO.2020.38.15_suppl.3550
58. Smyth E, Kouvelakis K, Cunningham D, Hahne JC, Peckitt C, Vlachogiannis G, et al. 646P EGFR amplification (amp) and survival in the REAL3 trial. Ann Oncol (2018) 29:282–030. doi: 10.1093/annonc/mdy282.030
59. Catenacci DVT, Lomnicki S, Chase L, Peterson B, Moore K, Markevicius U, et al. Personalized ANtibodies for GastroEsophageal Adenocarcinoma (PANGEA): Primary efficacy analysis of the phase II platform trial (NCT02213289). J Clin Oncol (2020) 38:356–6. doi: 10.1200/JCO.2020.38.4_suppl.356
60. Carneiro BA, Bestvina CM, Shmueli ES, Gan HK, Beck JT, Robinson R, et al. Phase I study of the antibody-drug conjugate ABBV-321 in patients with non-small cell lung cancer and squamous head and neck cancer with overexpression of the epidermal growth factor receptor. JCO (2020) 38:TPS3649–TPS3649. doi: 10.1200/JCO.2020.38.15_suppl.TPS3649
61. Lundy J, Marx GM, MacDiarmid J, Brahmbhatt H, Ganju V. Interim data: Phase I/IIa study of EGFR-targeted EDV nanocells carrying cytotoxic drug PNU-159682 (E-EDV-D682) with immunomodulatory adjuvant EDVs carrying α-galactosyl ceramide (EDV-GC) in patients with recurrent, metastatic pancreatic cancer. JCO (2020) 38:4632–2. doi: 10.1200/JCO.2020.38.15_suppl.4632
62. Park K, John T, Kim S-W, Lee JS, Shu CA, Kim D-W, et al. Amivantamab (JNJ-61186372), an anti-EGFR-MET bispecific antibody, in patients with EGFR exon 20 insertion (exon20ins)-mutated non-small cell lung cancer (NSCLC). JCO (2020) 38:9512–2. doi: 10.1200/JCO.2020.38.15_suppl.9512
63. Lum LG, Thakur A, Choi M, Deol A, Kondadasula V, Schalk D, et al. Clinical and immune responses to anti-CD3 x anti-EGFR bispecific antibody armed activated T cells (EGFR BATs) in pancreatic cancer patients. Oncoimmunology (2020) 9:1773201. doi: 10.1080/2162402X.2020.1773201
Keywords: esophageal cancer, gastric cancer, gastroesophageal cancer, epidermal growth factor receptor, cetuximab, panitumumab, targeted therapy, ctDNA
Citation: Maron SB, Xu J and Janjigian YY (2020) Targeting EGFR in Esophagogastric Cancer. Front. Oncol. 10:553876. doi: 10.3389/fonc.2020.553876
Received: 20 April 2020; Accepted: 05 November 2020;
Published: 08 December 2020.
Edited by:
Cornelis F. M. Sier, Leiden University, NetherlandsReviewed by:
Kei Muro, Aichi Cancer Center Hospital, JapanManidhar Reddy Lekkala, University of Rochester, United States
Copyright © 2020 Maron, Xu and Janjigian. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Steven B. Maron, marons@mskcc.org
 Steven B. Maron
Steven B. Maron James Xu
James Xu Yelena Y. Janjigian1
Yelena Y. Janjigian1